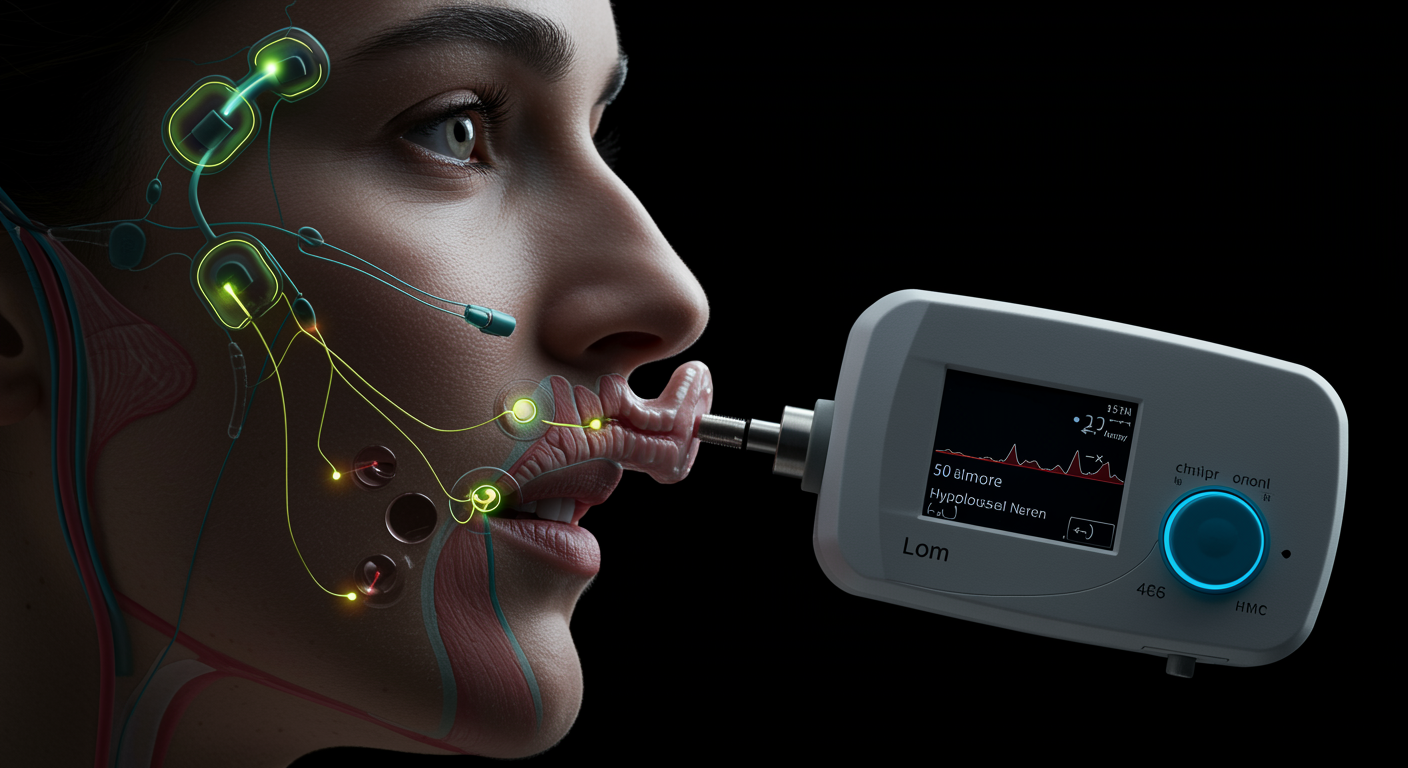
Clinical Practice Guidelines for Sleep Apnea and Snoring Treatment with Oral Appliances
What Do Clinical Guidelines Say About Oral Appliances for Sleep Apnea?
Updated clinical practice guidelines recommend oral appliance therapy as an effective first-line treatment for mild to moderate obstructive sleep apnea and primary snoring, with specific recommendations for patient selection, device types, and follow-up protocols. The guidelines, developed by the American Academy of Sleep Medicine and American Academy of Dental Sleep Medicine, establish that custom-fitted mandibular advancement devices are preferred over over-the-counter options, with effectiveness rates of 65-70% for reducing sleep apnea severity. The recommendations emphasize that oral appliances are particularly suitable for patients who cannot tolerate CPAP therapy, prefer a non-invasive treatment option, or have mild to moderate OSA without significant comorbidities.