Inside the Colonic Bioreactor: How S. boulardii Preserves Gut Anatomy During Antibiotics
Dr. Kumar’s Take
This study shows us that our gut health isn’t just about the type of microbes you have but where they live and how they’re arranged. The colon works like a layered factory called a bioreactor, and S. boulardii helps preserve its architecture during the upheaval caused by strong antibiotics. For patients, that spatial resilience may be what protects against lasting damage.
Key Takeaways
- Antibiotic treatment with ciprofloxacin + metronidazole suppresses many bacterial groups; most suppression occurs in the central fermentative region of the stool cylinder.
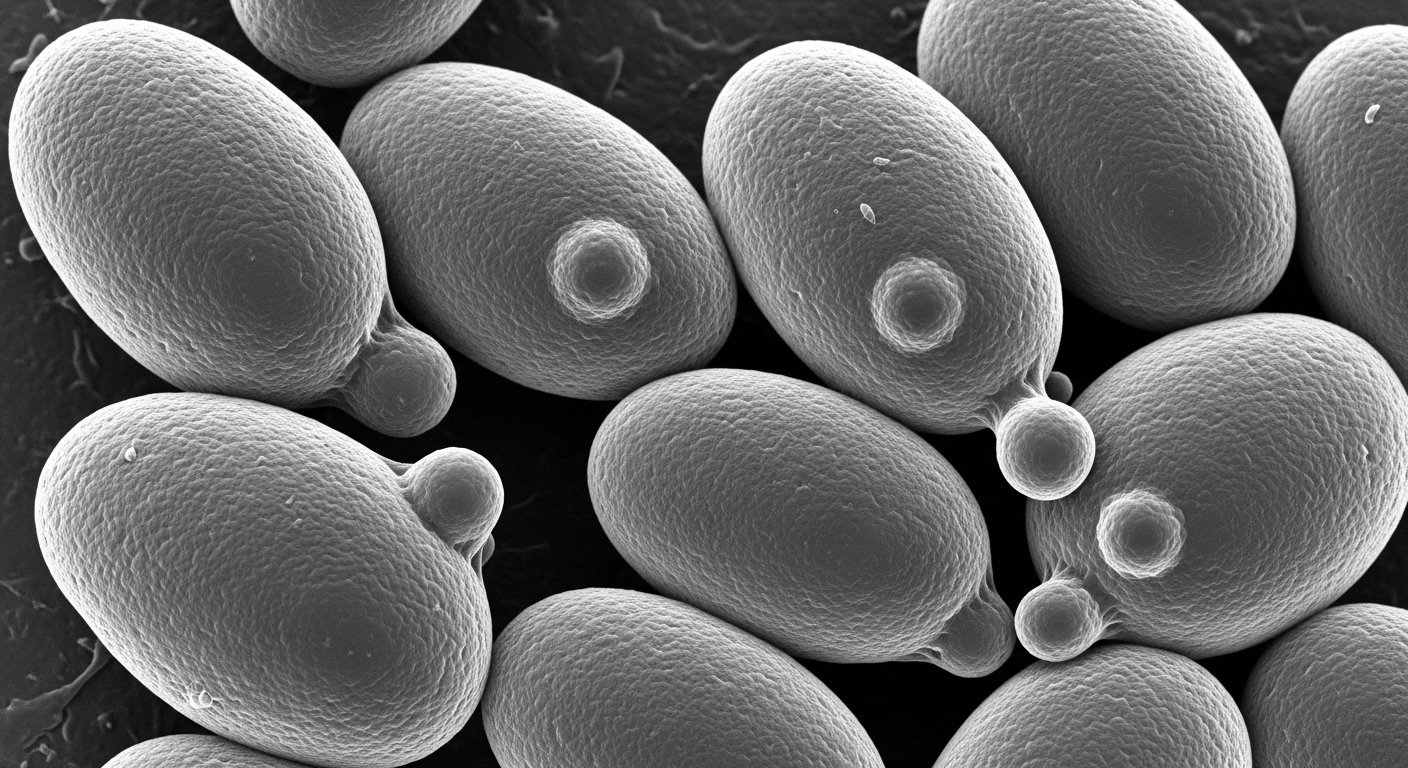
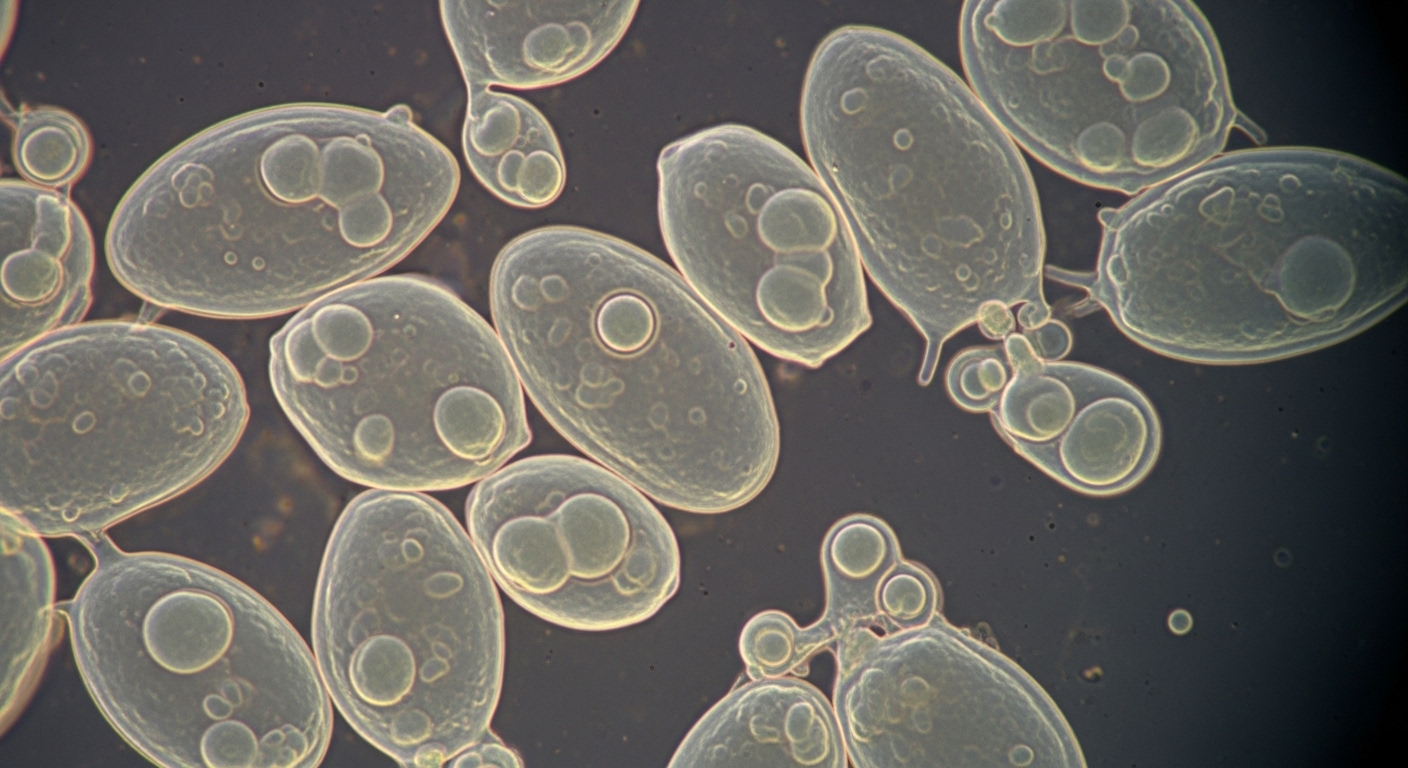
- There are three key zones in the “colonic bioreactor”: an outer mucus layer with almost no bacteria, a transitional mucus layer rich in bacteria, and a fermentation area inside largely filled with bacterial biomass and digestive leftovers.
- S. boulardii given concomitantly or prophylactically reduces antibiotic-induced suppression of “essential” bacterial groups (e.g. Faecalibacterium prausnitzii, Bacteroides, Roseburia).
- Recovery of bacterial diversity and biomass is much faster and more complete in S. boulardii‑treated groups, though even with probiotic treatment, full recovery takes months.
- Spatial location matters: the transitional layer acts like a refuge during antibiotic insult, and recovery tends to spring from there.
Actionable Tip
When prescribing strong antibiotics, consider starting Saccharomyces boulardii CNCM I‑745 at the same time. Supporting the structure of gut microbiota matters just as much as bacterial composition.