ACS Deep-Tank Fermentation: Pfizer's D-Day Production
How did Pfizer’s deep-tank fermentation revolutionize penicillin production?
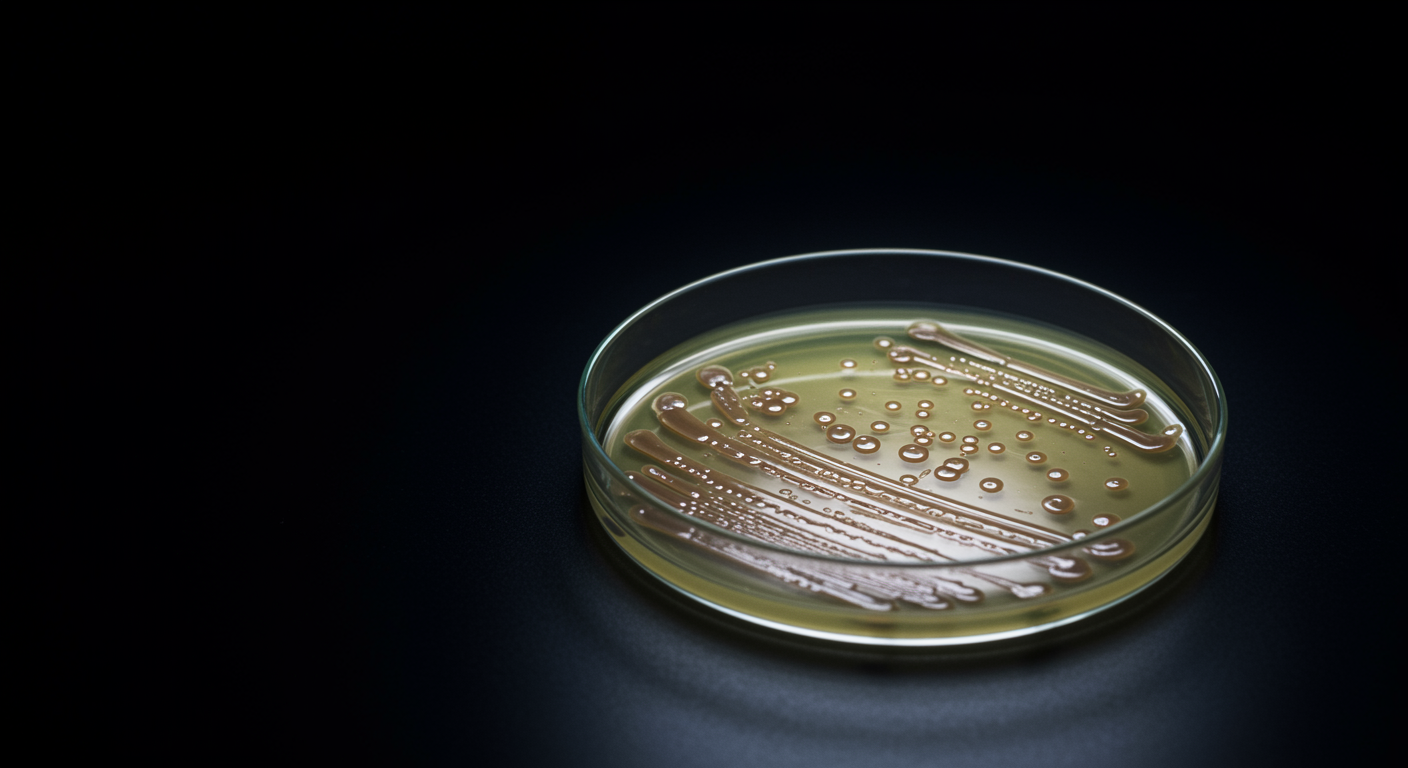
Pfizer’s adaptation of deep-tank fermentation from brewing technology enabled continuous, 24/7 penicillin production that increased yields by orders of magnitude and made D-Day supply possible. This industrial innovation transformed penicillin from laboratory curiosity to mass-produced medicine through engineering excellence.
The American Chemical Society’s commemorative booklet documents one of the most crucial industrial innovations in medical history. Pfizer’s deep-tank fermentation process replaced surface culture methods with submerged fermentation in large, continuously stirred and aerated tanks that could operate around the clock.