How Effective Is Upper Airway Stimulation as an Alternative to CPAP?
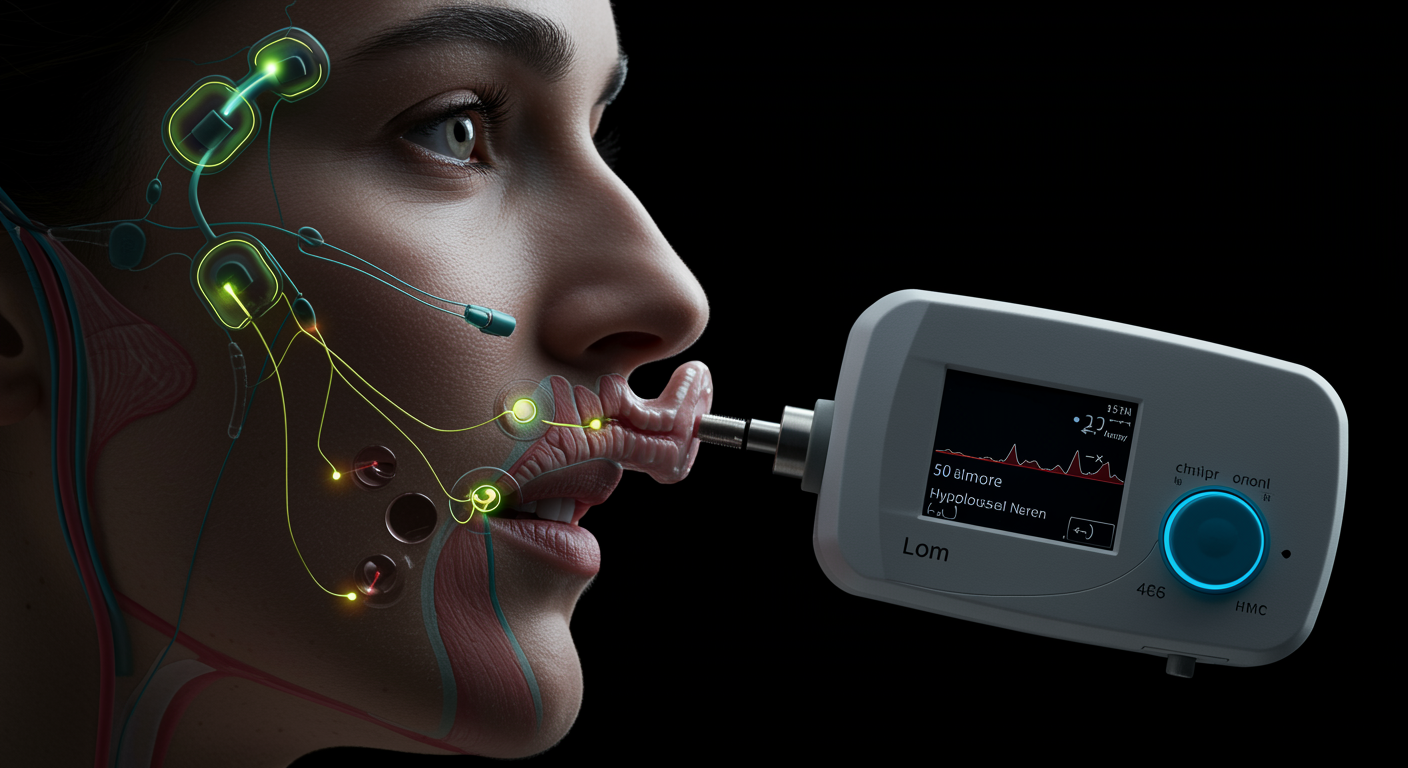
Upper airway stimulation (UAS) therapy provides a highly effective alternative to CPAP for treating obstructive sleep apnea, this landmark clinical trial demonstrates. The therapy, which uses an implanted device to stimulate the hypoglossal nerve and prevent airway collapse during sleep, reduced the apnea-hypopnea index (AHI) by 68% and significantly improved quality of life measures in patients who could not tolerate CPAP therapy. At 12 months, 66% of patients achieved treatment success (AHI reduction ≥50% and AHI <20 events/hour), with sustained benefits maintained over long-term follow-up. The therapy represents a breakthrough for the estimated 30-50% of sleep apnea patients who cannot use CPAP effectively.
Dr. Kumar’s Take
This research represents a game-changing advancement for sleep apnea treatment, particularly for the millions of patients who struggle with CPAP compliance. The 68% reduction in AHI is remarkable and clinically meaningful—that’s the kind of improvement that can dramatically reduce cardiovascular risk and improve quality of life. What’s particularly impressive is that these benefits are sustained over time, unlike many sleep apnea treatments that lose effectiveness. The mechanism is elegant: instead of using external pressure to keep airways open like CPAP, UAS works from the inside by stimulating the tongue muscle to maintain airway patency. While the surgery and device implantation represent significant interventions, for patients who have failed CPAP therapy, this offers genuine hope for effective treatment. The selection criteria are important—patients need to have moderate to severe OSA, BMI under 32, and specific anatomical characteristics—but for appropriate candidates, this can be life-changing. The technology continues to evolve, and I expect we’ll see even better outcomes as patient selection and device programming improve.
Key Findings
The STAR trial (Stimulation Therapy for Apnea Reduction) enrolled 126 patients with moderate to severe obstructive sleep apnea who had failed or could not tolerate CPAP therapy. At 12 months, upper airway stimulation therapy reduced the median AHI from 29.3 to 9.0 events per hour, representing a 68% improvement.
Treatment success, defined as AHI reduction of at least 50% and final AHI less than 20 events/hour, was achieved in 66% of patients. Quality of life measures showed significant improvements, with the Epworth Sleepiness Scale scores decreasing from 11.6 to 7.0, indicating substantial reduction in daytime sleepiness.
Oxygen desaturation events also improved dramatically, with the oxygen desaturation index decreasing by 70%. Bed partner assessments showed significant improvements in snoring and sleep disruption. Long-term follow-up data demonstrated sustained benefits over 5 years of therapy.
Brief Summary
The STAR trial was a prospective, multicenter study examining upper airway stimulation therapy in patients with moderate to severe obstructive sleep apnea who were intolerant of or had failed CPAP therapy. Participants underwent implantation of the Inspire UAS system, which consists of an implantable pulse generator, a sensing lead, and a stimulation lead connected to the hypoglossal nerve. The primary endpoints were AHI reduction and quality of life improvements at 12 months post-implantation.
Study Design
This was a prospective, single-arm trial with rigorous inclusion criteria including moderate to severe OSA (AHI 20-50), CPAP intolerance or failure, BMI ≤32, and absence of complete concentric collapse at the soft palate level on drug-induced sleep endoscopy. Patients underwent comprehensive sleep studies before and after implantation, with standardized device programming and optimization protocols. Long-term follow-up extended to 5 years to assess durability of treatment effects.
Results You Can Use
Upper airway stimulation reduces AHI by approximately 68% in appropriately selected patients, with two-thirds achieving clinically meaningful treatment success. The therapy significantly improves daytime sleepiness, with Epworth Sleepiness Scale scores dropping from moderate (11.6) to normal (7.0) ranges.
Quality of life improvements are substantial and sustained, with patients reporting better sleep quality, increased energy, and improved overall functioning. Bed partners report significant reductions in snoring and sleep disruption. The benefits are maintained over long-term follow-up, with 5-year data showing sustained efficacy.
Patient selection is crucial for success—candidates must have moderate to severe OSA, BMI under 32, and appropriate upper airway anatomy as determined by sleep endoscopy.
Why This Matters For Health And Performance
Upper airway stimulation provides a viable treatment option for the estimated 30-50% of sleep apnea patients who cannot effectively use CPAP therapy. This represents millions of people who previously had limited treatment options and remained at risk for cardiovascular complications, cognitive impairment, and reduced quality of life.
The therapy addresses a major gap in sleep apnea treatment, offering hope for patients who have struggled with CPAP compliance. The sustained long-term benefits suggest this can provide durable treatment for appropriately selected patients.
How to Apply These Findings in Daily Life
- Consider if CPAP has failed: UAS may be appropriate if you cannot tolerate CPAP despite optimization efforts
- Evaluate candidacy: Work with sleep specialists to determine if you meet selection criteria (moderate-severe OSA, BMI <32, appropriate anatomy)
- Understand the commitment: UAS requires surgical implantation and ongoing device management
- Seek experienced centers: Choose sleep centers with experience in UAS therapy and patient selection
- Plan for optimization: Device programming and adjustment may take several months to optimize
- Maintain follow-up: Regular monitoring is essential for long-term success with UAS therapy
Limitations To Keep In Mind
This study examined carefully selected patients who met specific criteria, and results may not apply to all sleep apnea patients. The therapy requires surgical implantation with associated risks and costs. Patient selection is crucial for success, and not all patients are appropriate candidates. Long-term device durability and the need for battery replacement over time require consideration.
Related Studies And Internal Links
- CPAP vs Oxygen for Sleep Apnea: Cardiovascular Outcomes
- Tirzepatide for Sleep Apnea and Obesity: Breakthrough Results
- CPAP Effects on Blood Pressure in Resistant Hypertension
- Sleep Apnea Screening: STOP-Bang Questionnaire Performance
- How to Sleep Better: Science Daily Playbook
FAQs
How does upper airway stimulation work?
UAS uses an implanted device to stimulate the hypoglossal nerve, which controls tongue movement. This stimulation prevents the tongue from collapsing backward and blocking the airway during sleep, maintaining airway patency without external pressure.
Who is a good candidate for upper airway stimulation?
Ideal candidates have moderate to severe OSA (AHI 20-50), have failed or cannot tolerate CPAP, have BMI ≤32, and lack complete concentric collapse at the soft palate level on sleep endoscopy. Careful evaluation by experienced sleep specialists is essential.
What are the risks and complications of UAS therapy?
Surgical risks include infection, bleeding, and device-related complications. Some patients may experience tongue weakness, speech changes, or device discomfort. Most complications are minor and resolve with time or device adjustment.
Conclusion
Upper airway stimulation therapy represents a breakthrough treatment for obstructive sleep apnea, reducing AHI by 68% and significantly improving quality of life in appropriately selected patients who cannot tolerate CPAP. This landmark trial establishes UAS as an effective long-term alternative for patients with moderate to severe OSA who meet specific selection criteria.