How did surgery go from 50% mortality to routine procedures?
The transformation of surgery from a last-resort procedure with 50% mortality rates to routine operations occurred through the systematic implementation of infection control measures, culminating in the antibiotic revolution. This century-long evolution made modern surgery possible by conquering the greatest threat to surgical patients: infection.
The journey from Lister's carbolic acid sprays in the 1860s to penicillin's arrival in the 1940s represents one of medicine's most dramatic transformations. What we heard in the penicillin podcast - that surgery was incredibly dangerous before antibiotics - understates the magnitude of this change. Infection wasn't just a complication; it was the primary cause of surgical death.This transformation happened in waves: antiseptic surgery, aseptic technique, and finally antimicrobial therapy. Each breakthrough built upon the previous, creating the foundation for modern surgical practice. The story shows how infection control evolved from crude chemical barriers to sophisticated understanding of microbial transmission and treatment.
What the data show:
- Mortality rates plummeted: Surgical mortality dropped from 45-50% in the pre-antiseptic era to under 5% by the mid-20th century
- Lister’s carbolic acid revolution: Antiseptic surgery reduced major amputation mortality from 45% to 15% in Lister’s early series
- Aseptic technique advanced further: Steam sterilization and sterile gloves reduced infection rates beyond what antiseptics alone could achieve
- Antibiotics completed the transformation: Penicillin and other antibiotics made previously impossible surgeries routine by providing treatment for inevitable infections
This comprehensive review traces surgical infection control from its origins through the antibiotic era, documenting how systematic approaches to preventing and treating infections revolutionized surgical practice and patient outcomes.
Dr. Kumar’s Take
This research perfectly captures the world that penicillin transformed. Before antibiotics, surgeons were essentially fighting a losing battle against infection using increasingly sophisticated but ultimately limited tools. Lister’s carbolic acid, sterile technique, and aseptic surgery were all crucial steps, but they could only prevent infection - they couldn’t treat it once it started.
What strikes me most is how this mirrors the pneumonia story we just covered. Just as pneumonia required complex state intervention programs before antibiotics, surgery required elaborate infection prevention rituals. Penicillin didn’t just add another tool - it fundamentally changed the risk-benefit calculation of surgery itself. Procedures that were too dangerous to attempt became routine because post-operative infections became treatable rather than fatal.
Historical Context
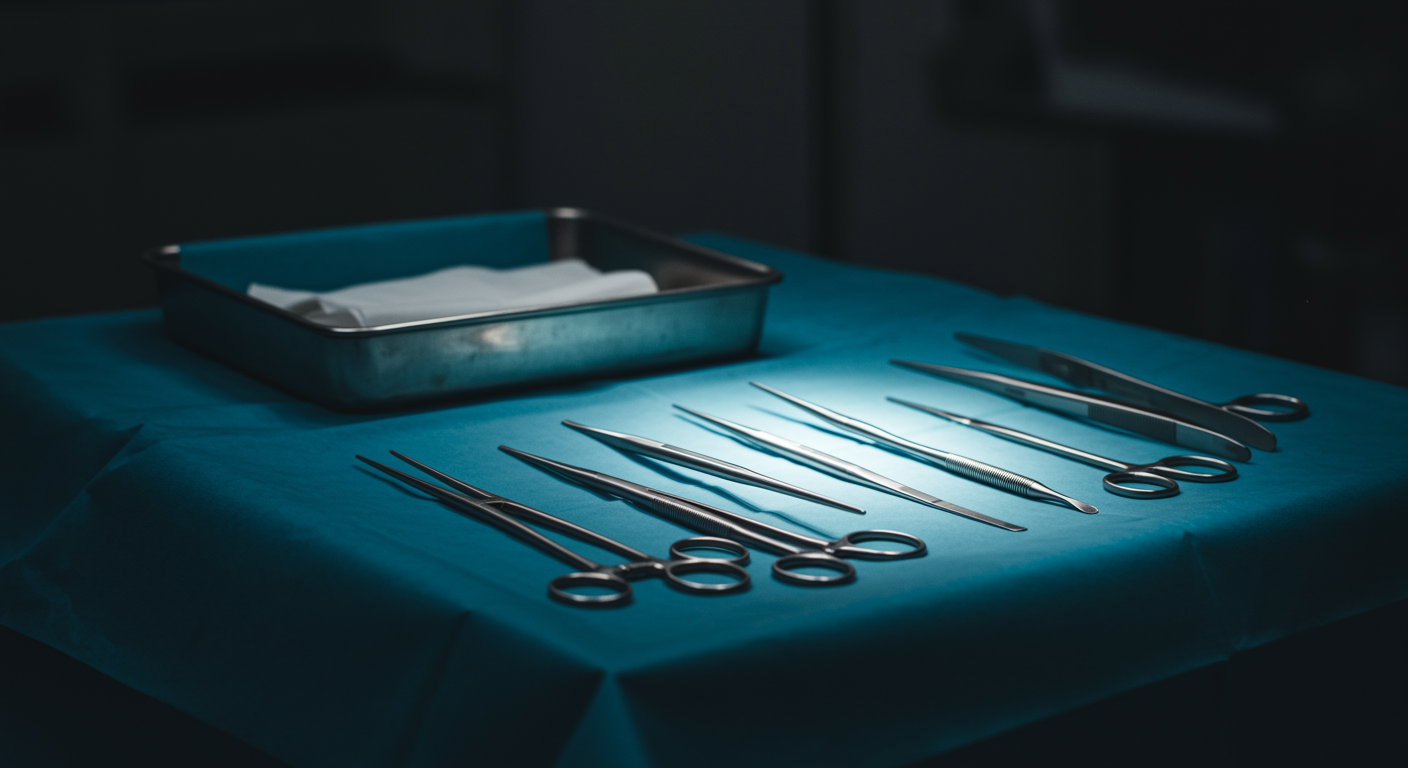
In the early 1800s, surgery was truly a last resort. The combination of no anesthesia and rampant infection made surgical mortality rates of 45-50% common. Even “successful” operations frequently ended in death from post-operative sepsis. Surgeons operated in street clothes, used unsterilized instruments, and had no understanding of microbial transmission.
The transformation began with Joseph Lister’s introduction of carbolic acid antisepsis in the 1860s, followed by the development of aseptic technique in the 1880s. Each advance reduced infection rates but couldn’t eliminate the fundamental problem: once infection occurred, treatment options remained extremely limited.
What the Research Shows
The evolution of surgical infection control occurred in three distinct phases, each building upon previous advances:
Phase 1: Antiseptic Surgery (1860s-1880s) Lister’s carbolic acid system created chemical barriers against infection. Operating theaters were sprayed with carbolic acid, instruments were soaked in antiseptic solutions, and wounds were dressed with carbolic-soaked materials. This reduced major amputation mortality from 45% to 15% in Lister’s series.
Phase 2: Aseptic Technique (1880s-1940s) Understanding of microbial transmission led to prevention-focused approaches: steam sterilization of instruments, sterile surgical gowns and gloves, and sterile operating environments. This further reduced infection rates and made more complex procedures feasible.
Phase 3: Antimicrobial Therapy (1940s onward) The arrival of sulfonamides and penicillin provided the missing piece: effective treatment for established infections. This didn’t just reduce mortality from existing procedures - it made entirely new categories of surgery possible by providing a safety net when prevention failed.
The Modern Era Contemporary surgery combines all three approaches: prevention through sterile technique, prophylactic antibiotics, and treatment of established infections. This layered approach has made surgical mortality rates below 1% routine for many procedures.
Practical Takeaways
- Prevention and treatment work synergistically: The most dramatic improvements came from combining infection prevention with effective treatment options
- Incremental progress builds transformative change: Each advance in infection control enabled the next, creating cumulative improvements
- Technology enables new possibilities: Antibiotics didn’t just improve existing surgeries - they made new procedures feasible
- Systematic approaches work: Coordinated infection control programs are more effective than isolated interventions
Related Studies and Research
- Penicillin: The Accidental Discovery That Changed Medicine and Won a War
- Ignaz Phillip Semmelweis’ Studies of Death in Childbirth
- Achievements in Public Health: Control of Infectious Diseases
- The Discovery of Penicillin: New Insights After More Than 75 Years
FAQs
Why was surgery so dangerous before infection control?
Without understanding microbial transmission, surgeons operated in contaminated environments with unsterilized instruments. Post-operative infections were nearly inevitable, and with no effective treatments available, mortality rates of 45-50% were common.
How did Lister’s carbolic acid system work?
Lister created chemical barriers against infection by spraying operating theaters with carbolic acid, soaking instruments in antiseptic solutions, and dressing wounds with carbolic-treated materials. This killed many bacteria and reduced infection rates significantly.
What’s the difference between antiseptic and aseptic technique?
Antiseptic technique uses chemicals to kill microorganisms, while aseptic technique prevents contamination through sterile environments and procedures. Aseptic technique proved more effective because it prevented exposure rather than trying to kill organisms after contact.
How did antibiotics change surgical practice?
Antibiotics provided effective treatment for post-operative infections, making surgery much safer. This didn’t just improve existing procedures - it made entirely new categories of surgery feasible by providing a safety net when infection prevention failed.
Bottom Line
The transformation of surgery from a desperate last resort to routine medical practice represents one of medicine’s greatest achievements. Through the systematic development of antiseptic surgery, aseptic technique, and antimicrobial therapy, surgical mortality dropped from 50% to under 1% for many procedures. This evolution shows how incremental advances in infection control can create revolutionary changes in medical practice, with antibiotics like penicillin providing the final breakthrough that made modern surgery possible.