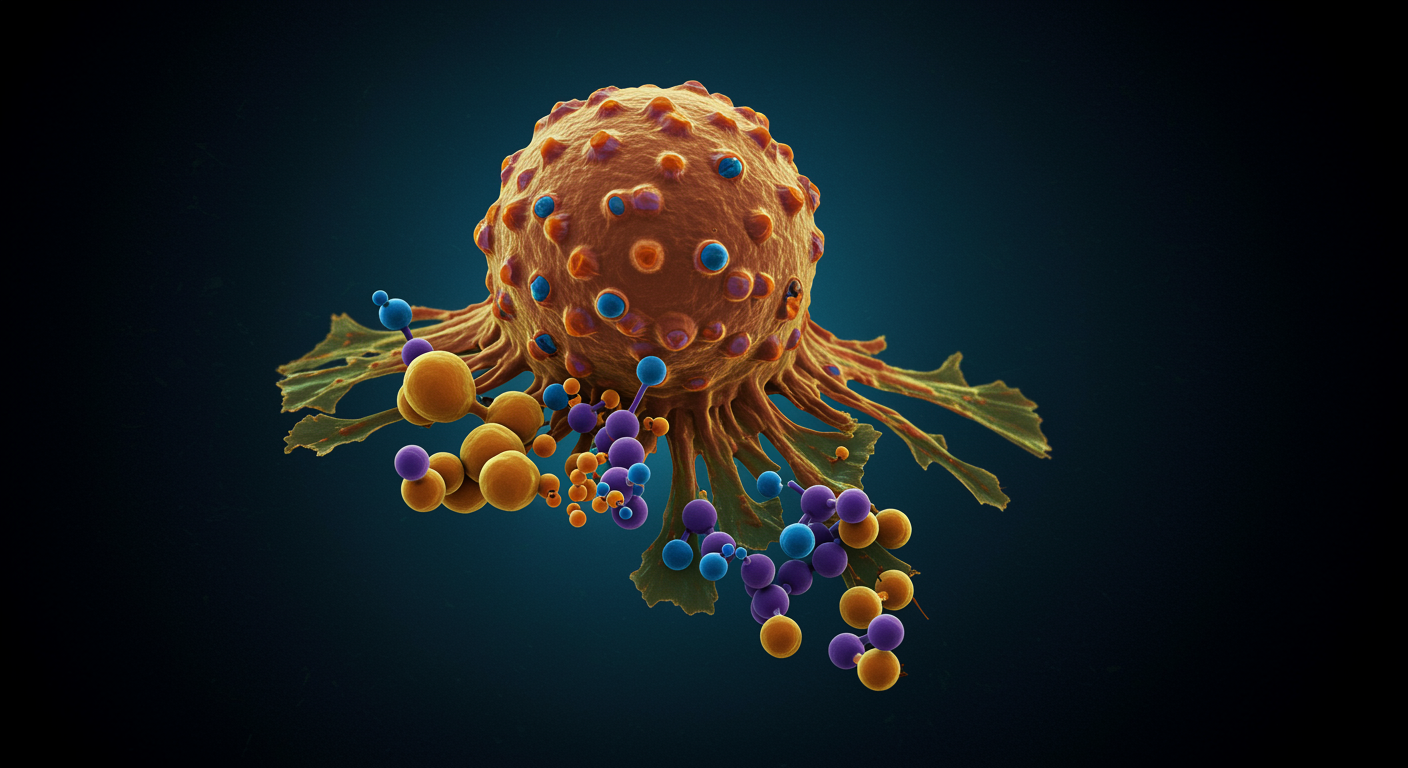
Can we target cancer’s sweet tooth for effective treatment?
Yes, researchers are developing multiple therapeutic strategies to exploit cancer cells’ dependence on glucose metabolism, though clinical success remains limited. Scientists have identified numerous targets along the glycolytic pathway, from glucose transporters to lactate exporters, with several compounds showing promise in early clinical trials.
Nearly a century after Otto Warburg first described cancer’s unusual metabolism, the Warburg effect has emerged as both a diagnostic tool and therapeutic target. Cancer cells’ preference for glucose fermentation creates unique vulnerabilities that researchers are learning to exploit through targeted interventions.
What the research shows:
- Multiple Targets Available: Scientists have identified therapeutic targets at every step of glycolysis, from glucose entry through lactate export
- Clinical Progress: MCT1 inhibitor AZD3965 reached Phase I trials and was well-tolerated at therapeutically effective doses
- Diagnostic Success: PET scans using glucose analogs have become standard practice for cancer detection and treatment monitoring
- Resistance Challenges: Cancer cells can switch to alternative metabolic pathways when glycolysis is blocked, limiting single-agent effectiveness
This comprehensive review from the International Journal of Molecular Sciences examines current therapeutic strategies targeting the Warburg effect, revealing both the promise and challenges of metabolic cancer therapy.
Dr. Kumar’s Take
Targeting cancer metabolism represents a fascinating shift from traditional chemotherapy approaches. Instead of directly attacking DNA or cell division, we’re essentially trying to starve cancer cells by disrupting their preferred energy source. The challenge lies in cancer’s metabolic flexibility - these cells have evolved sophisticated backup systems. The future likely lies in combination approaches that simultaneously target multiple metabolic pathways while enhancing immune system function.
Therapeutic Strategies in Development
Researchers have identified multiple intervention points along the glycolytic pathway, each offering unique advantages and challenges.
Glucose Transport Inhibitors represent the most upstream approach. Compounds like BAY-876 and KL-11743 block glucose entry into cells, effectively cutting off the fuel supply. These inhibitors have shown promise in triple-negative breast cancer models and can overcome chemotherapy resistance in gastrointestinal cancers.
Hexokinase Inhibitors target the first committed step of glycolysis. The classic compound 3-bromopyruvate has shown dramatic effects in preclinical studies but remains limited to case reports in humans due to safety concerns. 2-deoxyglucose, a glucose analog, showed early promise but clinical trials were discontinued due to hypoglycemia-like symptoms.
Lactate Pathway Targeting focuses on the end products of glycolysis. Lactate dehydrogenase inhibitors like FX11 and NHI-Glc-2 have demonstrated anti-tumor activity, while monocarboxylate transporter inhibitors prevent lactate export. The MCT1 inhibitor AZD3965 has progressed furthest in clinical development.
Tumor Microenvironment Impact
The Warburg effect profoundly shapes the tumor microenvironment through lactate accumulation and acidification. Tumor environments can reach lactate concentrations of 40 mM with pH dropping to 6.0-6.5, creating conditions that suppress immune function while promoting cancer progression.
This metabolic reprogramming affects multiple cell types within tumors. Tumor-associated macrophages are polarized toward pro-cancer phenotypes by lactate exposure. T-cells and natural killer cells lose their anti-tumor activity in high-lactate, low-pH environments. Meanwhile, regulatory T-cells remain functional, maintaining their immunosuppressive effects.
These observations have sparked interest in combining metabolic inhibitors with immunotherapy. Blocking glycolysis can restore glucose availability to immune cells while reducing immunosuppressive lactate levels, potentially enhancing checkpoint inhibitor effectiveness.
Clinical Challenges and Resistance
Despite promising preclinical results, translating Warburg effect inhibitors to clinical practice has proven challenging. The primary obstacle is that normal tissues also depend on glycolysis, particularly rapidly dividing cells and tissues lacking mitochondria like red blood cells.
Cancer cells have also evolved sophisticated resistance mechanisms. When one metabolic pathway is blocked, tumors can activate alternative energy sources including oxidative phosphorylation, acetate metabolism, or other fuel sources. This metabolic flexibility requires combination approaches targeting multiple pathways simultaneously.
The existence of multiple enzyme isoforms and transporters creates additional complexity. Blocking GLUT1 alone may not halt glucose uptake due to compensation by other glucose transporters. Similarly, inhibiting both MCT1 and MCT4 is required to effectively block lactate export.
Diagnostic Applications
While therapeutic applications remain challenging, the Warburg effect has found tremendous success in cancer diagnosis. PET scans using 18F-fluorodeoxyglucose (FDG) exploit cancer cells’ high glucose uptake for tumor detection and treatment monitoring.
Hyperpolarized 13C MRI represents an emerging technology that can directly visualize lactate production in real-time. This technique has shown success in prostate and breast cancer patients and may provide earlier detection of treatment response than conventional imaging.
Related Studies and Research
- Who Was Otto Warburg and Why Does His Cancer Research Still Matter?
- Why Do Cancer Cells Choose Inefficient Energy Production?
- How Does NAD+ Control Cancer’s Metabolic Switch?
- The Vitamin C Paradox: Beyond Scurvy to Cancer Treatment
FAQs
Why haven’t Warburg effect inhibitors become standard cancer treatment?
The main challenges are toxicity to normal tissues that also use glycolysis and cancer cells’ ability to switch to alternative metabolic pathways. Most single-agent approaches have shown limited clinical success, leading researchers toward combination strategies.
Which Warburg effect inhibitors are closest to clinical use?
The MCT1 inhibitor AZD3965 has progressed furthest, completing Phase I trials with acceptable safety profiles. Several glucose transport inhibitors are also in early clinical development.
Could dietary interventions target the Warburg effect?
Ketogenic diets and calorie restriction have shown promise in animal models by limiting glucose availability to tumors. Phase I trials in humans have demonstrated feasibility, but larger studies are needed to prove effectiveness.
How does targeting metabolism differ from traditional chemotherapy?
Traditional chemotherapy directly damages DNA or disrupts cell division, affecting all rapidly dividing cells. Metabolic targeting exploits cancer-specific metabolic dependencies, potentially offering better selectivity for tumor cells.
What role does the immune system play in metabolic therapy?
Lactate from cancer metabolism suppresses immune function. Blocking glycolysis can restore immune cell activity while reducing immunosuppressive signals, potentially enhancing immunotherapy effectiveness.
Bottom Line
Targeting the Warburg effect represents a promising but challenging approach to cancer therapy. While numerous compounds have shown preclinical success, clinical translation has been limited by toxicity concerns and cancer’s metabolic flexibility. The future likely lies in combination approaches that simultaneously target multiple metabolic pathways while enhancing immune function. Although therapeutic applications remain in development, the Warburg effect has already revolutionized cancer diagnosis through PET imaging and continues to provide insights into tumor biology that may unlock new treatment strategies.