Dr. Kumar’s Take:
A physiologic insight became a public health breakthrough. When glucose is present in the small intestine, it hitches a ride with sodium through SGLT1, pulling water into the body. That simple mechanism powers oral rehydration and helps stop dehydration from becoming deadly.
Key Takeaways:
✔ Glucose enables sodium absorption through SGLT1, and water follows.
✔ This mechanism explains why oral rehydration works during severe diarrhea.
✔ Electrolyte solutions with glucose outperform glucose-free formulas.
✔ Crane’s work laid the foundation for modern oral rehydration solution.
Brief Summary:
Question: Can a cellular transport mechanism translate into a lifesaving therapy for dehydration?
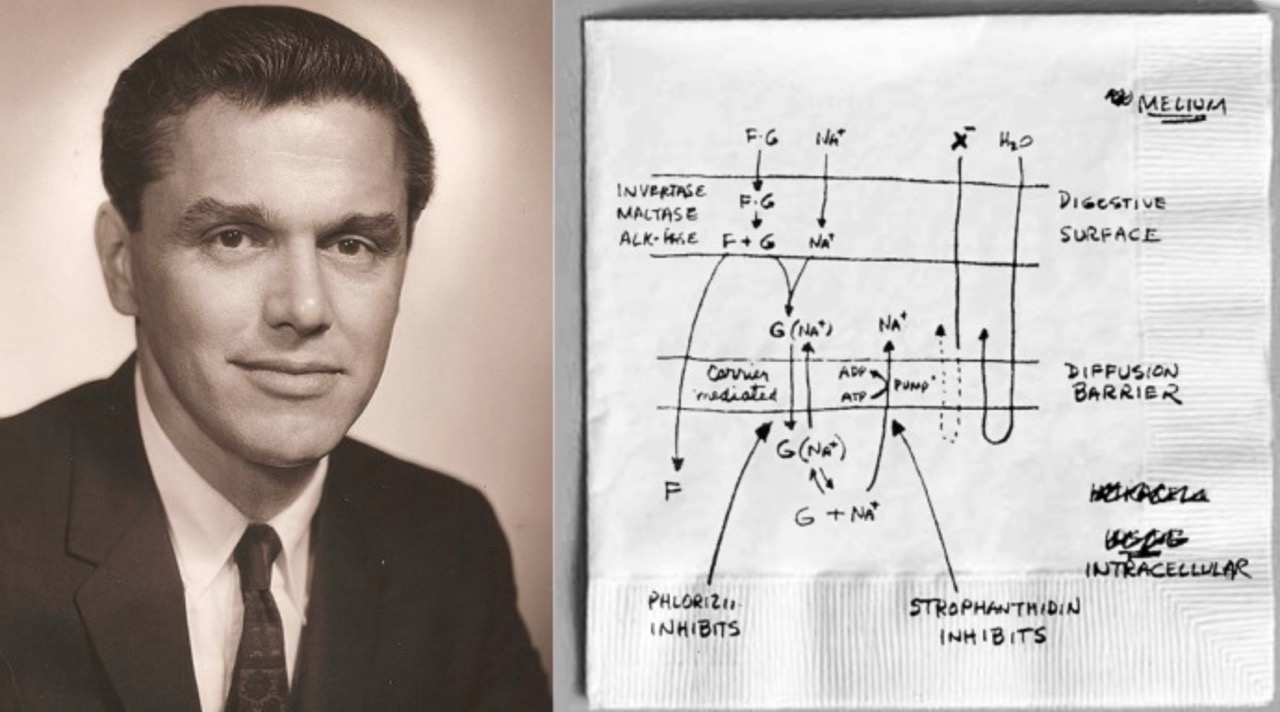
Mechanism: Sodium and glucose cotransport through SGLT1 increases sodium absorption.
Result: Sodium absorption draws water across the gut epithelium, restoring volume in diarrheal illness.
Impact: Forms the physiologic basis of WHO oral rehydration solution.
Population: Laboratory and physiologic studies summarized in a historical review.
Design: Narrative review of discovery and clinical application.
Primary outcomes: Mechanistic explanation and translation to therapy.
Study Design:
✔ Type: Historical and mechanistic review
✔ Measurements: Intestinal transport studies of sodium and glucose
✔ Analysis: Synthesis of transport findings and therapeutic implications
✔ Setting and timeframe: Mid-20th-century physiology through 2013 review
Results:
- SGLT1 couples glucose with sodium, enabling sodium absorption in the presence of glucose.
- Water follows osmotically when sodium is absorbed, improving hydration status.
- Glucose-free electrolyte solutions are inferior because they lack the cotransport effect.
- Physiology predicted clinical success later confirmed in cholera and childhood diarrhea.
How It Works (Biological Rationale):
- Glucose binds the transporter and opens the gate for sodium movement into enterocytes.
- Sodium uptake is linked to water movement from lumen to blood, improving hydration.
- The effect persists even when chloride secretion drives diarrhea, because SGLT1 remains functional.
- Proper osmolarity and sodium-glucose ratio make absorption efficient.
Related Studies and Research
Oral Maintenance Therapy for Cholera in Adults (1968 Lancet) – Early adult cholera data showing feasibility and safety of oral therapy.
Oral Fluid Therapy among Bangladesh Refugees – Field evidence in a humanitarian setting.
Fifty Years of Oral Rehydration Therapy – Perspective on global impact and evolution.
Oral Rehydration for Adults: Practical Treatment Guide – How to apply it at the bedside.
Podcast: The Simple Drink That Saved Millions: The Story of Oral Rehydration Solution
Frequently Asked Questions:
Why does adding glucose improve absorption?
Glucose engages SGLT1, which cotransports sodium into enterocytes. Water follows sodium, raising intravascular volume.
Can rehydration work if diarrhea is still ongoing?
Yes. Even when chloride secretion is high, SGLT1 remains active, so fluids keep moving from the gut into the body.
Do sports drinks work the same way?
Only if the sodium and glucose concentrations are in an effective range. Many off-the-shelf drinks are too low in sodium.
Conclusion:
A basic transport principle made a therapy simple, cheap, and scalable. Getting the ratio right allows glucose to carry sodium and water into the body and turns a deadly illness into a treatable condition.