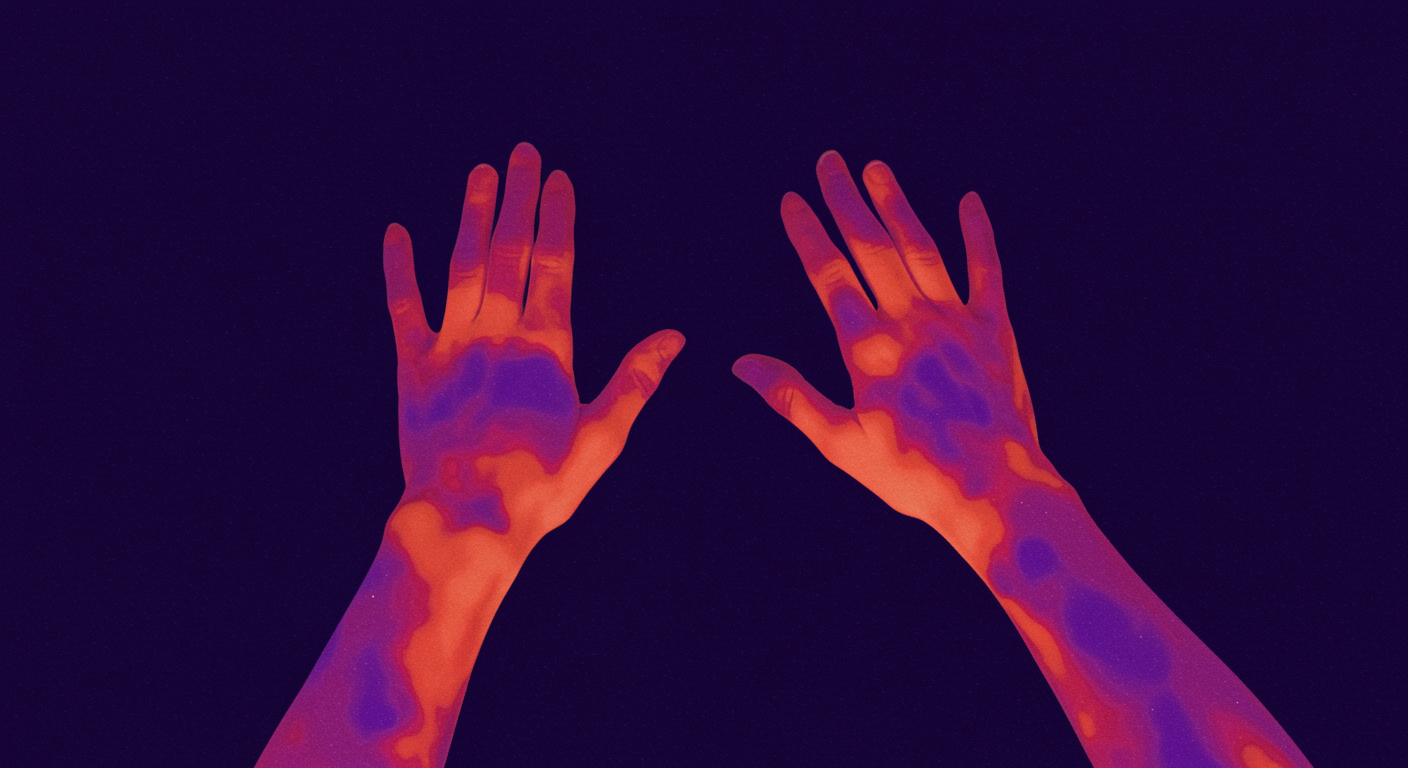
How Do Skin Temperature Changes Predict Sleep Onset Across Different Ages?
Skin temperature patterns, particularly in the hands and feet (distal skin temperature), serve as reliable predictors of sleep onset in young healthy adults, with warmer extremities indicating faster sleep initiation. However, this research reveals that aging and insomnia significantly alter these thermal patterns, with older adults and people with insomnia showing disrupted skin temperature regulation that correlates with longer sleep onset times. The study found that the normal evening rise in distal skin temperature that facilitates sleep onset becomes blunted or delayed in older adults and those with sleep disorders, suggesting that age-related changes in thermoregulation contribute to sleep difficulties.
Dr. Kumar’s Take
This research provides fascinating insight into why sleep becomes more difficult with age and why some people struggle with sleep onset. The finding that warm hands and feet predict faster sleep onset makes biological sense—peripheral vasodilation allows heat loss from the body’s core, which is necessary for the drop in core body temperature that triggers sleepiness. What’s particularly interesting is that this natural thermoregulatory process becomes impaired with aging and insomnia. Older adults often complain of cold hands and feet, and this research suggests this isn’t just a comfort issue—it may actually interfere with their ability to fall asleep efficiently. The practical implications are significant: warming the extremities before bedtime (through warm baths, socks, or other methods) may be especially helpful for older adults and people with insomnia. This also explains why some sleep hygiene recommendations like keeping the bedroom cool while warming the extremities can be so effective—it supports the natural thermoregulatory changes needed for sleep onset.
Key Findings
The study measured skin temperature at various body sites during the evening and found that distal skin temperature (hands and feet) increases significantly before sleep onset in young healthy adults, with warmer extremities predicting shorter sleep onset latency. This distal warming reflects peripheral vasodilation that facilitates heat loss and the drop in core body temperature necessary for sleep initiation.
However, aging significantly alters these patterns. Older adults showed reduced evening increases in distal skin temperature and weaker correlations between skin temperature and sleep onset timing. The normal thermal preparation for sleep becomes less pronounced and less predictive of actual sleep onset.
People with insomnia, regardless of age, also showed disrupted skin temperature patterns with delayed or blunted increases in distal skin temperature. The magnitude of distal skin temperature increase was smaller in insomniacs, and the timing was often delayed relative to their attempted bedtime.
Brief Summary
This study examined skin temperature patterns during the evening hours leading up to sleep in young adults, older adults, and individuals with insomnia. Participants wore temperature sensors at multiple body sites while their sleep onset was monitored using polysomnography or actigraphy. The research analyzed correlations between skin temperature changes and sleep onset latency across different age groups and sleep health conditions.
Study Design
The research used a controlled laboratory design with continuous skin temperature monitoring at multiple body sites (hands, feet, forehead, and torso) during evening hours leading to sleep. Sleep onset was objectively measured using polysomnographic or actigraphic methods. The study compared temperature patterns between young healthy adults, older adults, and individuals with diagnosed insomnia, controlling for environmental temperature and other factors that could influence thermoregulation.
Results You Can Use
In young healthy adults, warmer hands and feet in the evening predict faster sleep onset, with each degree of increase in distal skin temperature associated with significantly shorter sleep latency. The optimal pattern involves gradual warming of extremities beginning 1-2 hours before desired bedtime.
Older adults show reduced distal skin temperature increases and weaker correlations between skin temperature and sleep onset. This suggests that age-related changes in circulation and thermoregulation contribute to sleep difficulties in older populations.
People with insomnia show delayed and reduced distal skin temperature increases, indicating that thermal dysregulation may be both a cause and consequence of sleep difficulties. Interventions that promote peripheral warming may be particularly beneficial for this population.
Why This Matters For Health And Performance
Understanding the relationship between skin temperature and sleep onset provides a physiological basis for optimizing sleep hygiene practices. The research explains why certain interventions like warm baths, wearing socks to bed, or using heating pads for the extremities can be effective sleep aids, particularly for older adults and people with insomnia.
The findings also suggest that monitoring skin temperature patterns could potentially serve as an objective marker of sleep readiness and circadian timing, with applications for optimizing bedtime and identifying individuals at risk for sleep disorders.
How to Apply These Findings in Daily Life
- Warm your extremities before bed: Use warm socks, gloves, or heating pads to promote peripheral vasodilation
- Take warm baths or showers: The post-bath cooling effect combined with peripheral warming can facilitate sleep onset
- Time warming interventions: Begin warming hands and feet 1-2 hours before desired bedtime
- Consider age-related changes: Older adults may need more aggressive warming interventions due to reduced natural thermoregulation
- Monitor your patterns: Pay attention to whether cold hands and feet correlate with difficulty falling asleep
- Combine with cool environment: Keep the bedroom cool while warming extremities to support optimal thermoregulation
Limitations To Keep In Mind
This research examined relatively small groups and may not capture the full range of individual differences in thermoregulation. Environmental factors like room temperature and humidity can influence skin temperature patterns independent of sleep physiology. The study focused primarily on sleep onset and didn’t examine how skin temperature patterns affect sleep maintenance or sleep quality throughout the night.
Related Studies And Internal Links
- Sleep and Thermoregulation: Temperature’s Role in Sleep Quality
- The Temperature Dependence of Sleep: Optimal Conditions
- Passive Body Heating Before Bedtime Improves Sleep
- Age-Related Changes in Sleep Architecture and Hormones
- How to Sleep Better: Science Daily Playbook
FAQs
Why do warm hands and feet help with sleep onset?
Warm extremities indicate peripheral vasodilation, which allows heat loss from the body’s core. This core cooling is necessary to trigger the physiological changes that promote sleepiness and sleep onset.
Should I wear socks to bed if I have trouble falling asleep?
Based on this research, warming the extremities can be helpful for sleep onset, particularly for older adults or people with insomnia. However, avoid overheating, which can disrupt sleep later in the night.
Do these temperature patterns change throughout the night?
This study focused on sleep onset, but other research shows that skin temperature patterns continue to fluctuate throughout the night in coordination with sleep stages and circadian rhythms.
Conclusion
Skin temperature patterns, particularly warming of the hands and feet, predict sleep onset in young adults but become disrupted with aging and insomnia. Understanding these thermoregulatory changes provides a scientific basis for warming interventions that can facilitate sleep onset, especially in older adults and people with sleep difficulties.