Dr. Kumar’s Take
This clinical trial shows how Saccharomyces boulardii protects the gut microbiome during the assault of antibiotics. Healthy adults given amoxicillin‑clavulanate experience clear bacterial imbalances, but when Saccharomyces boulardii is added, the damage is far less severe. For those of us trying to preserve microbial resilience during antibiotic therapy, this type of evidence is gold.
Key Takeaways
- Four-arm study with healthy adult volunteers: S. boulardii alone, amoxicillin‑clavulanate alone, both combined, and no treatment.
- Antibiotic alone caused notable microbiota shifts, increasing potentially harmful bacteria like Escherichia and reducing beneficial ones like Roseburia.
- Adding S. boulardii blunted these effects and led to fewer GI symptoms.
- S. boulardii alone had no major impact on microbiota, showing its safety in healthy individuals.
- After stopping antibiotics, only partial microbiota recovery was seen by week two—unless S. boulardii was co-administered.
Actionable Tip
If you’re taking a course of antibiotics, include Saccharomyces boulardii CNCM I‑745 (500 mg twice daily) from day one until days after you finish antibiotics. It softens the microbial disruption and lowers the chance of GI side effects.
Study Summary
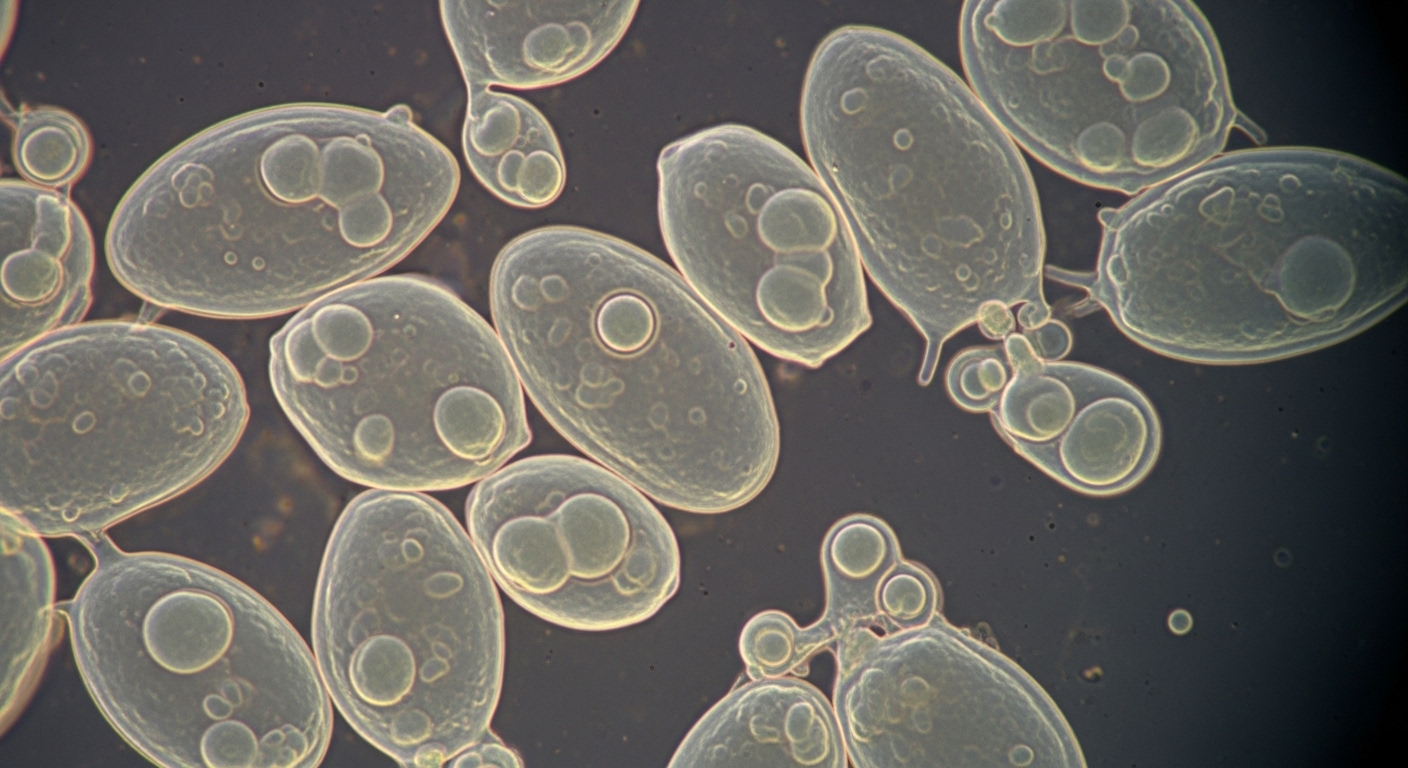
This randomized controlled trial assessed how S. boulardii, with or without antibiotics, influenced the gut microbiota of healthy adults. It used 16S rRNA sequencing to track bacterial genera and monitored GI symptoms. The goal was to understand how this probiotic could buffer antibiotic-induced dysbiosis.
Study Design
- Population: Healthy adult volunteers
- Groups:
- S. boulardii for 14 days
- Amoxicillin‑clavulanate for 7 days
- Combination of both
- No intervention
- Primary Outcomes: Changes in gut microbial composition and GI symptom scores
- Follow-up Duration: Two weeks after the intervention
Results
Antibiotic Alone Group:
- Increased abundance of Escherichia, Parabacteroides, Enterobacter
- Decrease in beneficial bacteria like Roseburia
- Higher diarrhea scores and GI discomfort
Antibiotic + S. boulardii Group:
- Smaller increases in potentially pathogenic genera
- Better GI symptom scores, fewer reports of diarrhea
- More favorable microbiota rebound after stopping treatment
S. boulardii Alone Group:
- No major change in gut flora compared to control
- No adverse effects reported
Recovery Pattern:
- In the antibiotic-only group, full microbial recovery had not occurred by day 14
- Co-administration with S. boulardii led to faster and more complete rebound
Biological Rationale
Saccharomyces boulardii resists destruction by antibiotics due to the fact that it’s a yeast. It competes with pathogenic organisms, supports commensal regrowth, and may suppress inflammation triggered by antibiotic-induced microbial shifts. By maintaining balance, it preserves both barrier function and microbial diversity.
Strengths & Limits
Strengths:
- Well-controlled, multi-arm design in healthy subjects
- Direct sequencing-based microbiome analysis
- Clear symptom reporting tied to microbiota shifts
Limitations:
- Small sample size limits generalizability
- Only one antibiotic tested
- Short follow-up (two weeks)
Related Studies and Research
- Saccharomyces boulardii in the prevention of antibiotic-associated diarrhoea: meta‑analysis
- Saccharomyces boulardii in the prevention of antibiotic-associated diarrhoea in children: RCT
- High‑Dose Vancomycin + SB for Recurrent C. difficile
- SB in H. pylori Therapy (RCT)
- 🎙️ Saccharomyces boulardii Explained – Podcast Episode
FAQ
Is this effect specific to amoxicillin-clavulanate?
This study focused on that antibiotic, but the mechanism suggests benefit across many broad-spectrum antibiotics.
Does S. boulardii alone affect healthy microbiomes?
No significant changes were seen. It appears safe and non-disruptive in healthy individuals.
Can this reduce the risk of C. difficile infection too?
While this study didn’t assess that directly, other studies have looked at that and shown that saccharomyces boulardii reduces recurrence of C. diff colitis.
Bottom Line
Saccharomyces boulardii CNCM I‑745 offers a simple way to reduce gut damage from antibiotics. It’s not a cure-all, but it preserves critical microbial species and improves tolerance. For patients starting antibiotics, it should be part of the standard protocol.