How do hormonal changes affect depression risk in women?
Hormonal changes across a woman’s reproductive life create vulnerable periods for depression by disrupting the hypothalamic-pituitary-adrenal (HPA) axis stress response system during puberty, menstruation, pregnancy, postpartum, and menopause. These fluctuations explain why women experience depression at twice the rate of men, with specific reproductive transitions creating windows of increased vulnerability.
What the data show:
- Female-to-male depression ratio: 2:1 ratio emerges after puberty, coinciding with HPA axis maturation
- Menstrual cycle vulnerability: 40% increased depression risk during luteal phase when progesterone drops
- Postpartum depression: 15-20% of women experience postpartum depression linked to dramatic HPA axis changes
- Perimenopause risk: Depression risk increases 2-4 times during perimenopause due to hormonal fluctuations
- HPA axis hyperactivity: Found in 60-80% of women with reproductive-related depression
- Vulnerable periods: Puberty, menstrual cycles, pregnancy, postpartum, and menopause all represent times of increased depression risk
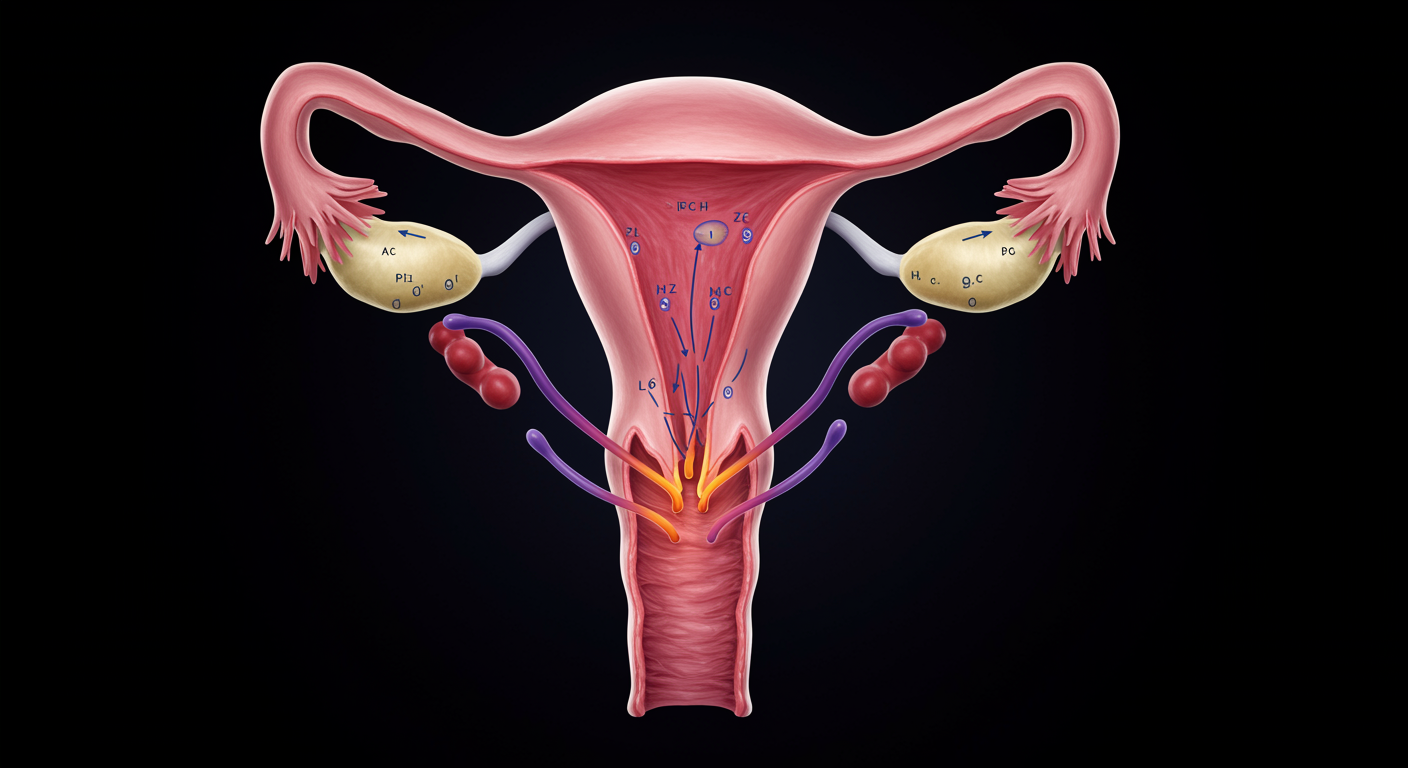
- Mechanism: Reproductive hormones (estrogen and progesterone) modulate the HPA axis stress response system - estrogen generally enhances stress resilience while progesterone withdrawal can trigger HPA hyperactivity, leading to excessive cortisol production; during reproductive transitions, rapid hormonal changes destabilize the HPA axis, creating windows of vulnerability for depression
Dr. Kumar’s Take
Understanding the HPA axis in women’s mental health is crucial for personalized depression care. The dramatic hormonal shifts women experience aren’t just “normal life events” - they represent real biological challenges to stress response systems that can trigger or worsen depression. This knowledge helps us time interventions better, choose appropriate treatments, and validate women’s experiences of mood changes during reproductive transitions.
What the Research Shows
Research consistently demonstrates that HPA axis function varies significantly across women’s reproductive stages, with each transition presenting unique challenges for mental health. The interplay between reproductive hormones (estrogen, progesterone) and stress hormones (cortisol) creates complex patterns of depression vulnerability that differ markedly from men’s more stable hormonal environment.
Study Snapshot
This comprehensive review analyzed HPA axis function across different reproductive stages in women, examining cortisol patterns, stress reactivity, and depression risk during puberty, menstrual cycles, pregnancy, postpartum period, and menopause. The analysis included both cross-sectional and longitudinal studies tracking hormonal and mood changes over time.
Results in Real Numbers
Key findings about HPA axis and women’s depression:
- 2:1 female-to-male depression ratio emerges after puberty, coinciding with HPA axis maturation
- 40% increased depression risk during luteal phase of menstrual cycle when progesterone drops
- 15-20% of women experience postpartum depression linked to dramatic HPA axis changes
- Perimenopause increases depression risk by 2-4 times due to hormonal fluctuations
- HPA axis hyperactivity found in 60-80% of women with reproductive-related depression
How This Works (Biological Rationale)
The HPA axis regulates stress response through a complex cascade involving the hypothalamus, pituitary gland, and adrenal glands. Reproductive hormones modulate this system - estrogen generally enhances stress resilience while progesterone withdrawal can trigger HPA hyperactivity. During reproductive transitions, rapid hormonal changes can destabilize the HPA axis, leading to excessive cortisol production and increased depression vulnerability.
Why This Matters for Health and Performance
Understanding HPA axis changes across reproductive stages helps explain:
- Timing of depression onset in women often coincides with hormonal transitions
- Treatment response variations based on reproductive stage and hormone levels
- Symptom patterns that may fluctuate with menstrual cycles or life stages
- Prevention opportunities during high-risk reproductive transitions
- Personalized treatment approaches based on individual hormonal profiles
Practical Takeaways
- Track mood patterns in relation to menstrual cycles to identify hormonal influences
- Anticipate vulnerable periods during reproductive transitions and plan support accordingly
- Consider hormone-informed treatments that account for reproductive stage and HPA axis function
- Support stress management during high-risk periods like postpartum and perimenopause
- Validate hormonal influences on mood rather than dismissing them as “just hormones”
- Collaborate with reproductive health specialists for comprehensive care during transitions
Related Studies and Research
Episode 31: Depression Explained — The Biology Behind the Darkness
Episode 32: Depression Recovery Roadmap: A Step-by-Step, Evidence-Based Plan
FAQs
Why are women more susceptible to depression than men?
The 2:1 female-to-male depression ratio largely stems from hormonal influences on the HPA axis during reproductive years. Estrogen and progesterone fluctuations create periods of vulnerability that men don’t experience.
Can hormone therapy help with depression during reproductive transitions?
Hormone therapy may help some women, particularly during perimenopause, but should be carefully considered with healthcare providers as benefits and risks vary individually.
How can women prepare for high-risk periods like postpartum or menopause?
Preparation includes stress management skills, social support systems, monitoring for early symptoms, and establishing relationships with mental health providers before transitions occur.
Bottom Line
The HPA axis undergoes significant changes across women’s reproductive lifecycle, creating windows of depression vulnerability during hormonal transitions. Understanding these patterns enables better prevention, earlier intervention, and more personalized treatment approaches for women’s mental health.