How do omega-3 fatty acids restore gut-brain balance in depression?
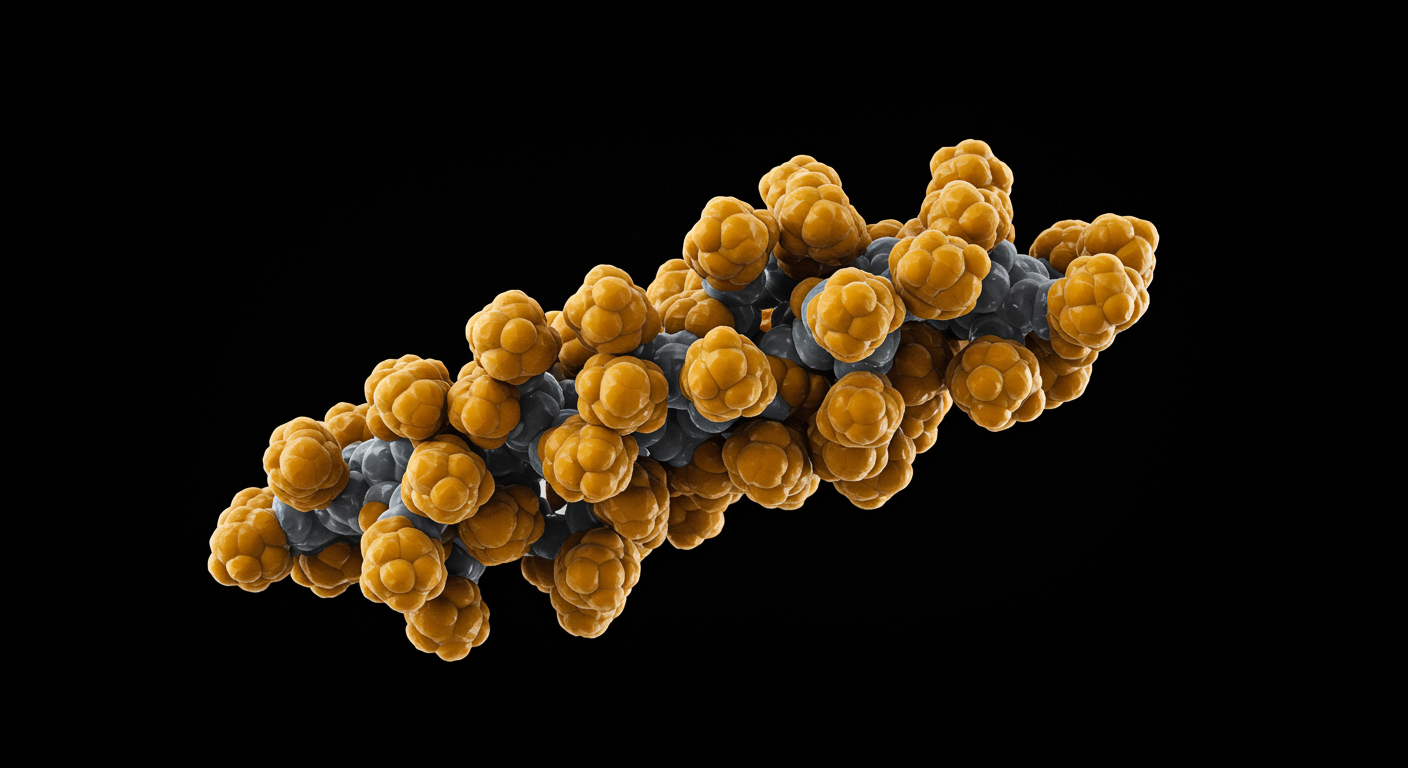
Omega-3 fatty acids restore gut-brain axis balance by promoting beneficial gut bacteria, reducing inflammation, and enhancing neural plasticity through multiple interconnected pathways. A comprehensive review published in Nutrients synthesizes evidence showing that EPA and DHA work as network modulators, addressing dysregulation across immune, neural, and metabolic systems that contribute to depression.
Omega-3 fatty acids work by reshaping gut microbiota composition to increase beneficial bacteria like Bifidobacterium and Lactobacillus, strengthening intestinal barrier integrity to reduce inflammation, promoting specialized pro-resolving mediators that actively resolve inflammation, supporting neurogenesis and BDNF production for brain plasticity, and modulating the HPA axis to reduce stress reactivity.
What the data show:
- Gut microbiome: Omega-3s increase beneficial bacteria (Bifidobacterium, Lactobacillus) and SCFA-producing genera (Blautia, Bacteroides, Roseburia, Coprococcus) while reducing pro-inflammatory bacteria
- Inflammation: EPA supplementation increases specialized pro-resolving mediators and reduces pro-inflammatory cytokines (TNF-α, IL-1β, IL-6) in patients with depression
- Neuroplasticity: DHA supports neurogenesis, increases BDNF levels, and enhances dendritic spine density and synaptic plasticity
- Stress response: Omega-3 supplementation reduces cortisol responses to stress and normalizes HPA axis function
- Oxidative stress: Omega-3s reduce lipid peroxidation and enhance antioxidant capacity, with stronger effects in individuals with elevated baseline oxidative stress
A comprehensive review published in Nutrients synthesizes evidence from multiple studies demonstrating that omega-3 polyunsaturated fatty acids act as network modulators, restoring balance across the gut-brain axis and interconnected biological pathways to improve depression through their multifaceted effects on microbiota, inflammation, neuroplasticity, and stress regulation.
Dr. Kumar’s Take
This review beautifully illustrates why omega-3 fatty acids are so effective for depression - they don’t just work on one pathway, they restore balance across multiple interconnected systems. The gut-brain axis is fascinating because it shows how our digestive system directly communicates with our brain through the vagus nerve, immune system, and metabolic pathways. When this communication breaks down, depression can result. Omega-3s help restore this balance by reducing inflammation, supporting beneficial gut bacteria, improving neurotransmitter production, and enhancing neural plasticity. This systems-level approach explains why omega-3s can be so effective when other single-target treatments fail.
Study Snapshot
This comprehensive review analyzed the role of omega-3 polyunsaturated fatty acids in restoring balance across multiple biological systems involved in depression, with particular focus on the gut-brain axis. The researchers examined how EPA and DHA influence gut microbiome composition, intestinal barrier function, immune system regulation, neurotransmitter synthesis, and neural plasticity. The review synthesized evidence from multiple disciplines to understand omega-3s’ multifaceted therapeutic mechanisms.
Results in Real Numbers
This comprehensive review synthesized evidence from multiple studies examining how omega-3 fatty acids restore gut-brain axis balance and improve depression through interconnected pathways. For gut microbiome effects, omega-3 supplementation increases beneficial bacteria including Bifidobacterium and Lactobacillus, which are known to reduce intestinal inflammation and support barrier function. Omega-3s also promote the expansion of short-chain fatty acid (SCFA)-producing genera such as Blautia, Bacteroides, Roseburia, and Coprococcus, which produce butyrate, acetate, and propionate that reinforce epithelial tight junctions and reduce intestinal permeability. In animal models of stress-induced depression, omega-3 supplementation restored disrupted Firmicutes/Bacteroidetes ratios and increased beneficial Ruminococcaceae abundance, demonstrating their ability to reverse stress-induced gut dysbiosis.
For anti-inflammatory effects, EPA supplementation in patients with major depressive disorder increases circulating specialized pro-resolving mediators (SPMs) including resolvins and maresins in a dose- and time-dependent fashion. These SPMs actively terminate inflammation by reducing NF-κB activation, downregulating pro-inflammatory cytokines like TNF-α, IL-1β, and IL-6, and limiting inflammasome activation. In adolescents with depression, lower levels of maresin-1 were associated with greater symptom severity, and these levels normalized with treatment. The review also highlighted that omega-3s modulate tryptophan metabolism, suppressing the inflammatory kynurenine pathway and promoting serotonin biosynthesis, which helps restore serotonergic tone while limiting neurotoxic kynurenine derivatives.
For neuroplasticity and stress regulation, omega-3 supplementation increases brain-derived neurotrophic factor (BDNF) levels in children and adolescents with depression, with higher baseline n-6 to n-3 ratios associated with lower BDNF concentrations. In animal models, omega-3s preserve hippocampal neurogenesis, increase dendritic spine density, and restore BDNF-TrkB signaling even under inflammatory conditions. For stress response, 12 weeks of EPA and DHA supplementation (2.4 grams per day) significantly reduced morning salivary cortisol in adolescents with depression, with higher baseline cortisol associated with greater symptom severity. In middle-aged adults, four months of high-dose omega-3 supplementation (2.5 grams per day) markedly attenuated cortisol responses to laboratory stressors, while eight weeks of omega-3 treatment (1.2 grams per day) reduced cortisol awakening response in employees with clinical burnout. For oxidative stress, omega-3 supplementation reduces lipid peroxidation in both plasma and cell membranes while enhancing antioxidant capacity, with stronger antidepressant responses observed in individuals with elevated baseline oxidative stress and sufficient plasma EPA+DHA reserves.
Who Benefits Most
Individuals with depression who also have digestive issues, inflammatory conditions, or metabolic dysfunction may benefit most from omega-3’s multi-system approach. People with treatment-resistant depression may find omega-3s valuable because they address multiple pathways simultaneously rather than targeting single mechanisms.
Patients interested in addressing root causes of depression rather than just symptoms may benefit from omega-3s’ ability to restore balance across interconnected biological systems. Individuals with depression and concurrent gut health issues may be particularly responsive to omega-3 therapy.
Safety, Limits, and Caveats
While omega-3 fatty acids are generally safe, the review noted that therapeutic effects depend on achieving adequate tissue levels of EPA and DHA, which may require several months of consistent supplementation. Individual responses vary based on baseline omega-3 status, genetic factors, and overall health.
The quality and bioavailability of omega-3 supplements vary significantly between products, affecting therapeutic outcomes. The review emphasized that omega-3s work best as part of comprehensive approaches that also address diet, lifestyle, and other factors affecting gut-brain axis function.
Practical Takeaways
- Understand that omega-3s work through multiple interconnected pathways, making them particularly valuable for complex conditions like depression
- Consider omega-3 supplementation as part of a comprehensive approach that also addresses gut health, inflammation, and overall nutrition
- Choose high-quality omega-3 supplements with verified EPA and DHA content, and be patient as therapeutic effects may take several months to develop
- Focus on supporting overall gut-brain axis health through diet, stress management, and lifestyle factors alongside omega-3 supplementation
- Discuss omega-3 therapy with healthcare providers who can assess your individual needs and monitor progress across multiple systems
What This Means for Depression Treatment
This review establishes omega-3 fatty acids as multi-system therapeutic agents that address the complex, interconnected nature of depression rather than targeting single pathways. The findings support integrating omega-3s into comprehensive treatment approaches that consider gut-brain axis function.
The research also validates the importance of nutritional psychiatry and systems-based approaches to mental health that address root causes rather than just symptoms.
Related Studies and Research
EPA Supplementation: Pro-Resolving Lipid Mediators Key to Response
Episode 31: Depression Explained — The Biology Behind the Darkness
Episode 32: Depression Recovery Roadmap: A Step-by-Step, Evidence-Based Plan
FAQs
How do omega-3s affect the gut-brain axis?
Omega-3s promote beneficial gut bacteria, improve intestinal barrier function, reduce inflammation, and enhance communication between the gut and brain through multiple pathways including the vagus nerve.
Why are omega-3s more effective than single-target treatments for some people?
Omega-3s work through multiple interconnected systems simultaneously, addressing the complex, multifactorial nature of depression rather than targeting single pathways.
How long does it take for omega-3s to restore gut-brain axis balance?
The review suggests that meaningful changes in gut-brain axis function may take several months of consistent omega-3 supplementation to achieve therapeutic tissue levels.
Bottom Line
Omega-3 polyunsaturated fatty acids restore balance across multiple interconnected biological pathways including the gut-brain axis, immune system, and neural networks, making them powerful therapeutic agents for depression that address root causes rather than just symptoms.