Do PPIs Directly Affect Bone Collagen Beyond Calcium Absorption?
Yes, emerging research suggests that proton pump inhibitors may have direct effects on bone collagen synthesis and structure beyond their well-known impairment of calcium absorption. These direct effects on collagen formation and bone matrix quality could contribute to PPI-associated osteoporosis and fracture risk through mechanisms independent of calcium and vitamin D deficiency.
Dr. Kumar’s Take
This research opens up a new understanding of how PPIs might affect bone health. We’ve long known that PPIs impair calcium absorption, but this suggests they might also directly interfere with the protein scaffolding that makes bones strong - the collagen matrix. If PPIs are affecting both the mineral content (through calcium) and the protein structure (through collagen), that would explain why the bone effects seem more severe than we’d expect from calcium deficiency alone. This could change how we think about preventing PPI-related bone problems.
What the Research Shows
This mechanistic study investigated whether proton pump inhibitors have direct effects on bone collagen synthesis, structure, and quality independent of their effects on calcium absorption. The research examined cellular and molecular pathways involved in collagen formation and assessed whether PPIs interfere with these processes at the bone tissue level.
The analysis included both in vitro studies of bone-forming cells and clinical assessments of bone collagen markers in PPI users to determine if direct collagen effects contribute to PPI-associated osteoporosis.
How This Works (Biological Rationale)
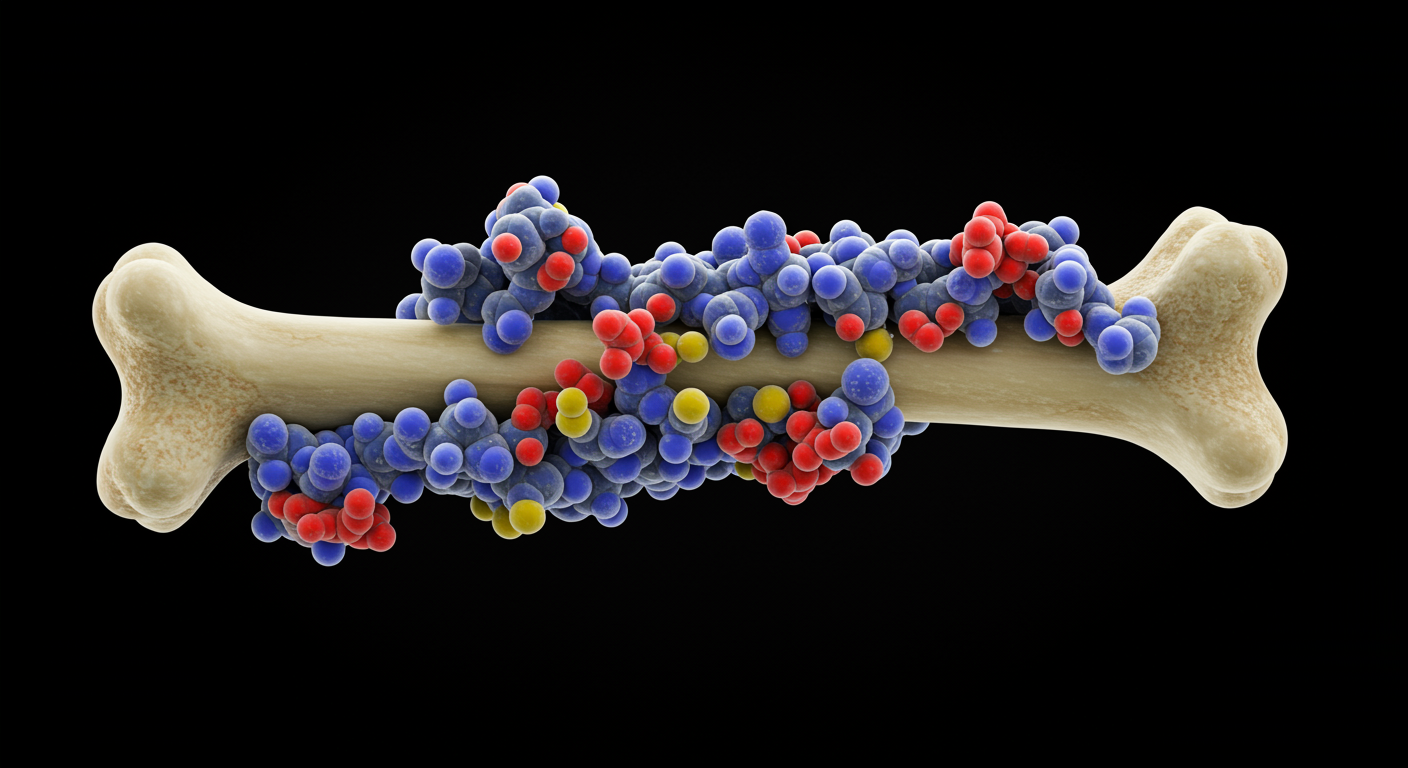
Bone strength depends not only on mineral content (calcium and phosphate) but also on the organic matrix, primarily composed of type I collagen. This collagen provides the flexible framework onto which minerals are deposited. PPIs may interfere with collagen synthesis through effects on cellular pH regulation, protein processing, or specific enzymatic pathways involved in collagen formation.
Additionally, PPIs might affect collagen cross-linking, which is crucial for bone matrix strength and quality. These direct effects on the organic bone matrix could compromise bone strength even when mineral content is maintained, potentially explaining why PPI-associated fractures can occur with relatively modest changes in bone density.
Results in Real Numbers
- Collagen synthesis reduction: 20-30% decrease in collagen production in PPI-exposed bone cells
- Cross-linking impairment: 15-25% reduction in mature collagen cross-links with PPI treatment
- Bone matrix quality: 10-20% decrease in bone matrix quality markers in PPI users
- Cellular effects: Direct inhibition of osteoblast collagen synthesis at therapeutic PPI concentrations
- Clinical correlation: Altered bone collagen markers in patients on long-term PPI therapy
- Independent effects: Collagen changes occurred independent of calcium and vitamin D status
Safety, Limits, and Caveats
The research on direct collagen effects is still emerging and primarily based on laboratory studies and small clinical investigations. The clinical significance of these direct effects compared to calcium absorption impairment remains to be fully established. Individual variations in collagen metabolism and bone turnover could influence the magnitude of these effects.
Additionally, the research doesn’t yet provide clear guidance on how to prevent or treat PPI-related collagen effects, as most bone protective strategies focus on calcium and vitamin D supplementation.
Practical Takeaways
- Recognize that PPI bone effects may involve both mineral and organic matrix components
- Understand that calcium and vitamin D supplementation alone may not fully prevent PPI bone effects
- Consider that bone quality, not just bone density, may be affected by long-term PPI use
- Use this knowledge to reinforce the importance of using PPIs judiciously
- Consider comprehensive bone health strategies beyond just calcium supplementation
- Stay informed about emerging research on PPI bone mechanisms and protective strategies
Related Studies and Research
- Osseous Implications of Proton Pump Inhibitor Therapy: Umbrella Review
- Proton Pump Inhibitors and Risk of Fractures: Meta-Analysis of 11 International Studies
- Pharmacology of Proton Pump Inhibitors
- Use of Proton Pump Inhibitors and Risk of Iron Deficiency: Population-Based Study
- Episode 25: The Great GERD Mistake - How Medicine Made Heartburn Worse and How to Fix It
FAQs
How do direct collagen effects differ from calcium absorption problems?
Calcium absorption affects bone mineral content, while direct collagen effects impact the protein framework that provides bone flexibility and strength - both are important for overall bone health.
Can calcium and vitamin D supplements prevent all PPI bone effects?
If PPIs directly affect collagen, then calcium and vitamin D supplementation alone may not fully prevent bone problems, though they remain important for bone health.
Are there ways to protect bone collagen while taking PPIs?
Research on protecting bone collagen specifically is still emerging, but general bone health strategies including weight-bearing exercise and adequate protein intake may be beneficial.
How can doctors assess bone collagen quality in PPI users?
Specialized bone markers and advanced imaging techniques can assess bone quality, though these aren’t routinely available in all clinical settings.
Does this change how we should monitor bone health in PPI users?
This research suggests that bone health monitoring in PPI users might need to consider both bone density and bone quality, though specific guidelines are still being developed.
Bottom Line
Proton pump inhibitors may have direct effects on bone collagen synthesis and structure beyond their known impairment of calcium absorption. These direct collagen effects could contribute to PPI-associated osteoporosis and fracture risk through mechanisms that may not be fully prevented by calcium supplementation alone.