Can Oxygen Therapy Improve Cancer Treatment?
Yes. This review from Expert Review of Anticancer Therapy explains how tumor oxygenation inhibits cancer growth and enhances the effects of chemoradiotherapy. The authors propose that combining oxygen therapy with immunotherapy could create a highly effective approach to cancer treatment.
Tumors often grow faster than their blood supply, creating regions of low oxygen (hypoxia). This hypoxic environment helps cancer cells survive and resist treatment. Oxygenating tumors may reverse these advantages.
Key Findings
Why Hypoxic Tumors Are More Dangerous:
- Hypoxic (low-oxygen) tumor environments contribute to cancer progression
- Cancer cells shift their metabolism in ways that help them survive low oxygen
- These metabolic changes weaken the tumor’s antioxidant defenses
- Hypoxic tumors resist standard treatments more effectively
How Oxygen Therapy Is Delivered:
- Water-soluble ozone therapy
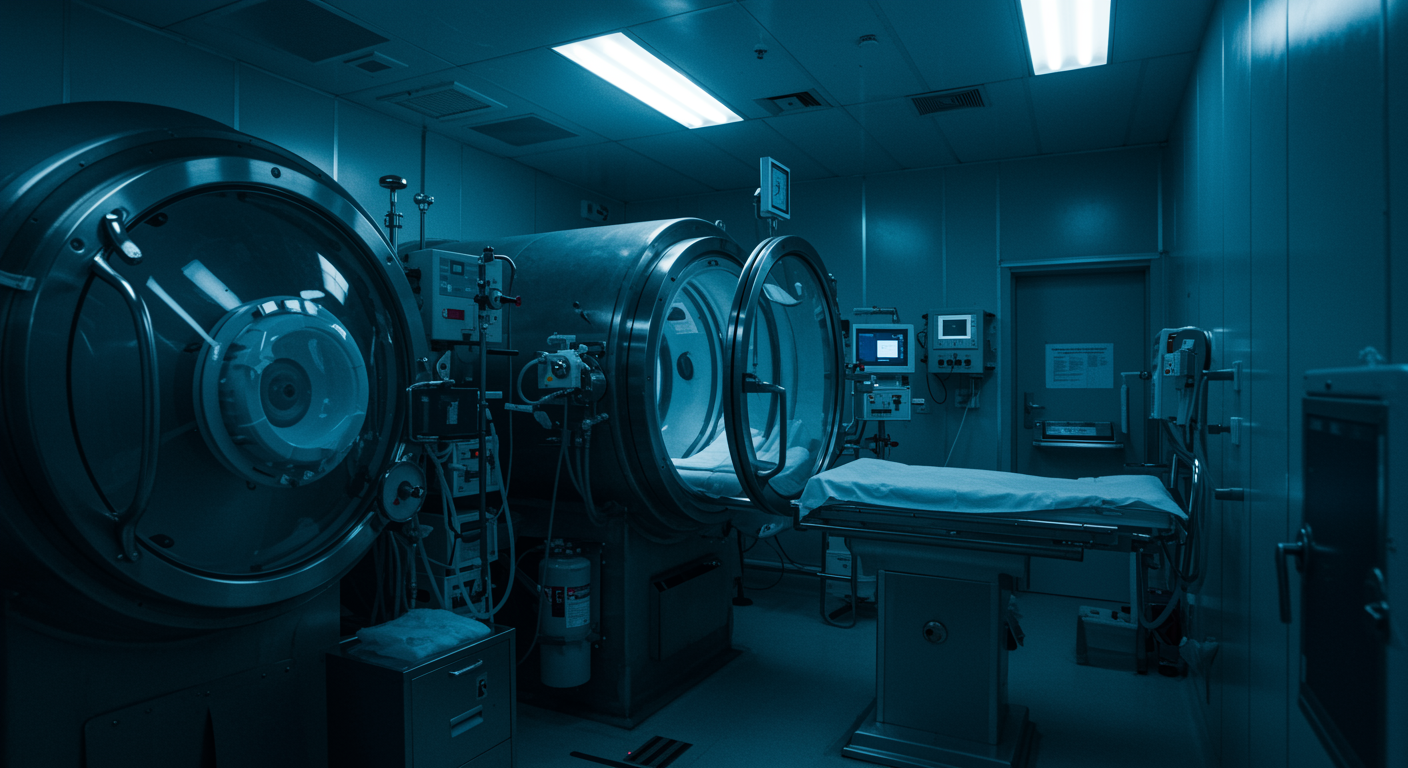
- Hyperbaric oxygen therapy (HBOT)
What Tumor Oxygenation Accomplishes:
- Inhibits tumor growth
- Enhances anti-tumor effects of chemoradiotherapy
- Potentiates blood vessel occlusion therapies
- Improves outcomes in both animal experiments and clinical settings
The Immunotherapy Connection: Reactive oxygen species (ROS) powerfully influence both innate and adaptive immunity. The researchers propose combining oxygen therapy with:
- Immune checkpoint inhibitors
- Drug-induced immunostimulation
- Adoptive cell therapy
- Hyperthermia (heat therapy)
Dr. Kumar’s Take
This perspective article highlights an underappreciated aspect of cancer treatment: the importance of tumor oxygen levels. The logic is straightforward. Cancer cells in hypoxic environments are harder to kill. Oxygenating these tumors removes a key survival advantage.
What excites me most is the proposed combination with immunotherapy. We know reactive oxygen species affect immune cell function. By combining oxygen therapy with checkpoint inhibitors or adoptive cell therapy, we might achieve synergistic effects. The authors suggest this could maximize anticancer effects while minimizing side effects.
The key insight from the article’s highlights deserves emphasis: oxidative stress-induced ROS can preferentially damage tumor cells without significantly affecting normal cells. This selectivity is crucial for any cancer therapy.
The Science Explained Simply
Why Tumors Become Hypoxic: Tumors grow rapidly. They quickly outgrow their blood supply. Without adequate blood vessels, oxygen can’t reach the center of the tumor mass. These hypoxic regions become sanctuaries where cancer cells survive treatments.
How Cancer Cells Adapt: Cancer cells switch to a different metabolism (increased glycolysis, hampered Krebs cycle). This allows them to survive on less oxygen but weakens their ability to handle oxidative stress.
Why Oxygen Therapy Helps: When you deliver high concentrations of oxygen, these adapted cancer cells face a challenge they’re not prepared for. Their weakened antioxidant defenses make them vulnerable to the reactive oxygen species that oxygen therapy generates.
Combining with Other Treatments
With Chemoradiotherapy: Both chemotherapy and radiation work better when tumors are well-oxygenated. Many cancer-killing mechanisms require oxygen. Hypoxic regions resist these treatments.
With Blood Vessel Occlusion: Some treatments try to cut off the tumor’s blood supply. Oxygen therapy may enhance these effects by supporting healthy tissue while stressing adapted cancer cells.
With Immunotherapy: This is where the authors see the most promise. Immune cells need to function properly to attack tumors. Oxygen levels affect immune cell activity. The combination could produce “maximal anticancer effects with minimal side effects.”
Practical Takeaways
- Tumor hypoxia contributes to cancer progression and treatment resistance
- Oxygen therapy can inhibit tumor growth in animal and clinical studies
- Hyperbaric oxygen therapy is the main clinical method for tumor oxygenation
- Combining oxygen with chemoradiotherapy enhances anti-tumor effects
- Oxygen therapy combined with immunotherapy shows theoretical promise
- ROS can preferentially damage tumor cells while sparing normal cells
Related Studies and Research
- EWOT and Precancerous Skin Lesions
- Effect of Hypoxia and Hyperoxia on Exercise Performance
- Oxygen Therapy During ADL Rehabilitation in COVID-19
- Oxidative Stress, Mitochondrial Dysfunction, and Aging
FAQs
How does oxygen therapy kill cancer cells?
Oxygen therapy works by generating reactive oxygen species (ROS) in the tumor. Cancer cells that have adapted to low-oxygen environments have weakened antioxidant defenses. This makes them more vulnerable to ROS-induced damage than normal cells. Additionally, many standard treatments (chemotherapy, radiation) work better when tumors are well-oxygenated.
Is hyperbaric oxygen therapy used for cancer now?
Hyperbaric oxygen therapy is FDA-approved for certain uses, including helping radiation injuries heal. Its use specifically to enhance cancer treatment is still being studied. The approach described in this article, combining HBOT with immunotherapy, represents a future direction rather than current standard practice.
Could oxygen therapy replace chemotherapy?
No. This review discusses oxygen therapy as an adjunct to conventional treatments, not a replacement. The authors propose combining oxygen therapy with chemoradiotherapy and immunotherapy to enhance their effects. It should be considered a potential addition to comprehensive cancer treatment, not a standalone cure.
Bottom Line
This review from Expert Review of Anticancer Therapy makes a compelling case for oxygen therapy in cancer treatment. Tumor oxygenation inhibits cancer growth and enhances the effects of chemoradiotherapy in both animal experiments and clinical settings. The authors propose that combining oxygen therapy with immunotherapy could create a “highly-effective clinical biological approach to cancer treatment” by leveraging the profound influence of reactive oxygen species on both innate and adaptive immunity. While more clinical research is needed, the theoretical framework for oxygen-enhanced cancer therapy is well-supported.