How Does Obesity Compromise the Gastroesophageal Junction?
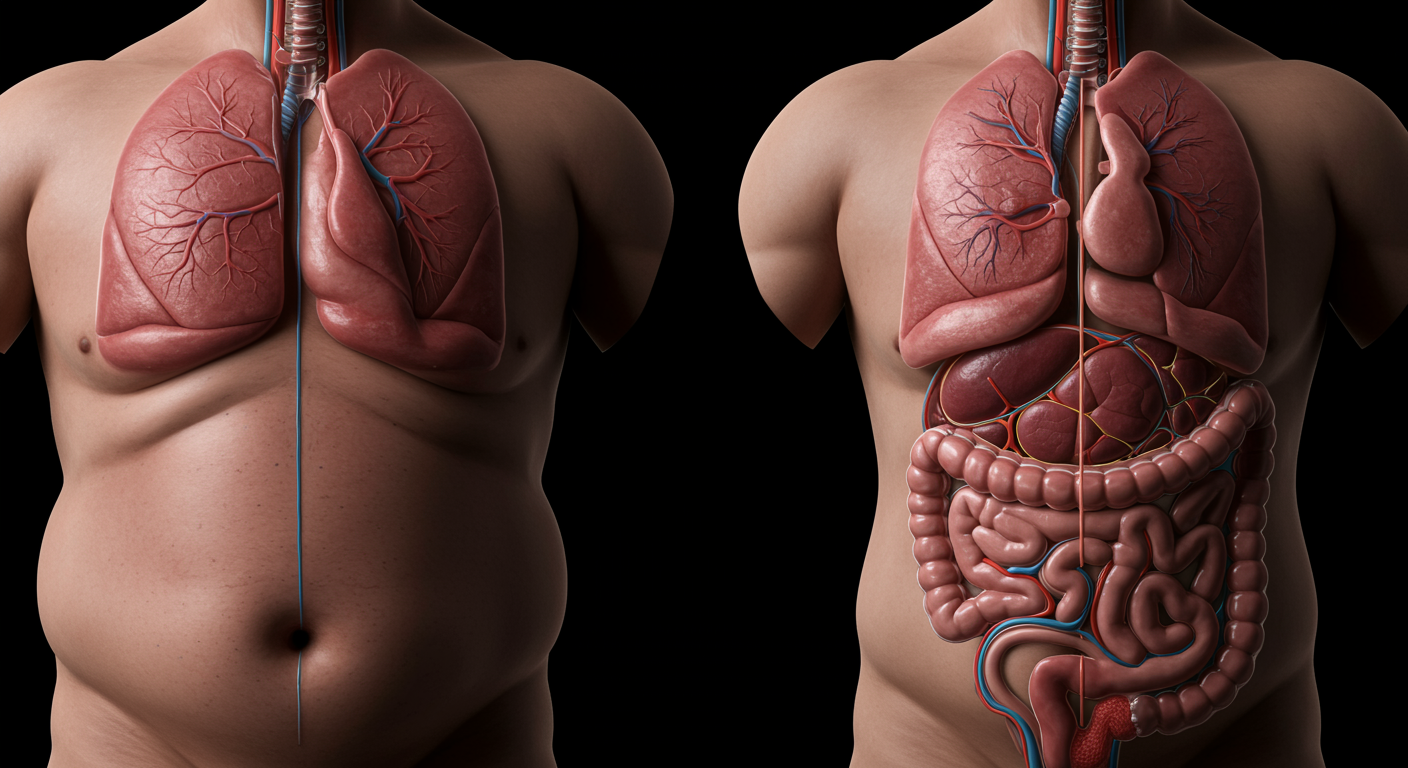
Obesity poses a significant challenge to esophagogastric junction integrity by increasing intra-abdominal pressure, altering anatomical relationships, and disrupting the normal anti-reflux mechanisms that prevent gastric contents from entering the esophagus. These mechanical and physiological changes create a cascade of effects that progressively weaken the gastroesophageal junction’s ability to maintain an effective barrier against reflux.
Dr. Kumar’s Take
This research explains why obesity is such a powerful risk factor for GERD - it literally changes the anatomy and mechanics of the gastroesophageal junction. The increased abdominal pressure from excess weight acts like a constant squeeze on the stomach, pushing contents upward while simultaneously compromising the very structures designed to prevent reflux. It’s a perfect storm where the problem (increased pressure) overwhelms the solution (anti-reflux mechanisms). Understanding this helps explain why weight loss can be so dramatically effective for GERD patients.
What the Research Shows
This comprehensive analysis examined how obesity affects the structural and functional integrity of the gastroesophageal junction through multiple mechanisms. The research included anatomical studies, pressure measurements, and clinical assessments to understand how excess weight progressively compromises the anti-reflux barrier.
The study demonstrated that obesity creates a cascade of changes at the gastroesophageal junction that collectively overwhelm the body’s natural defenses against reflux, leading to progressive deterioration of junction integrity with increasing weight.
How This Works (Biological Rationale)
Obesity increases intra-abdominal pressure through excess visceral fat, creating a pressure gradient that constantly pushes gastric contents toward the esophagus. This increased pressure also affects the crural diaphragm, which normally provides additional support to the lower esophageal sphincter.
The anatomical changes include alteration of the angle of His, displacement of the gastroesophageal junction, and potential development or worsening of hiatal hernia. These structural changes reduce the effectiveness of both the intrinsic sphincter mechanism and the extrinsic support provided by surrounding structures.
Results in Real Numbers
- Pressure increase: 50-100% higher intra-abdominal pressure in obese vs. normal weight individuals
- Junction displacement: 2-3 cm proximal migration of gastroesophageal junction with severe obesity
- Sphincter pressure reduction: 25-40% decrease in lower esophageal sphincter pressure
- Hiatal hernia prevalence: 3-fold higher incidence in obese patients
- Angle of His alteration: 30-50 degree change in gastroesophageal angle with obesity
- Reflux episode increase: 200-300% more reflux episodes in severely obese patients
Safety, Limits, and Caveats
The research examined anatomical and physiological changes but may not fully capture individual variations in anatomy, genetic factors, or the complex interactions between different obesity-related mechanisms. The studies also focused primarily on mechanical effects and may not address all aspects of how obesity affects gastroesophageal junction function.
Additionally, the research didn’t extensively examine the reversibility of these changes with weight loss or the time course of anatomical restoration following significant weight reduction.
Practical Takeaways
- Recognize that obesity creates multiple simultaneous challenges to gastroesophageal junction integrity
- Understand that weight loss addresses the root mechanical cause of junction compromise
- Appreciate that even modest weight loss may provide significant benefits for junction function
- Consider that severely obese patients may need more intensive GERD treatment approaches
- Realize that bariatric surgery may provide both weight loss and anatomical benefits for the gastroesophageal junction
- Use this knowledge to motivate comprehensive weight management in obese GERD patients
Related Studies and Research
- Obesity Increases Esophageal Acid Exposure
- Association Between Obesity and GERD: A Review of the Epidemiological Evidence
- Clinical Significance of Hiatal Hernia
- Hiatal Hernia, Lower Esophageal Sphincter and Their Combined Effect
- Episode 25: The Great GERD Mistake - How Medicine Made Heartburn Worse and How to Fix It
FAQs
Can weight loss restore gastroesophageal junction integrity?
While research suggests that significant weight loss can improve junction function and reduce reflux, the extent of anatomical restoration may vary based on the degree and duration of obesity.
How much weight loss is needed to improve junction function?
Studies suggest that losing 10-15% of body weight can provide meaningful improvements in gastroesophageal junction function and GERD symptoms.
Are the anatomical changes from obesity permanent?
Many obesity-related changes appear to be at least partially reversible with significant weight loss, though complete restoration may not always occur, especially with long-standing severe obesity.
Does the type of obesity (central vs. peripheral) affect junction integrity differently?
Central obesity appears particularly problematic for gastroesophageal junction integrity due to greater effects on intra-abdominal pressure and anatomical relationships.
Should obese GERD patients be considered for bariatric surgery?
Bariatric surgery may provide both weight loss and potential anatomical benefits for the gastroesophageal junction, though decisions should be individualized based on overall health status and GERD severity - discuss options with your healthcare provider.
Bottom Line
Obesity compromises gastroesophageal junction integrity through multiple mechanical and anatomical mechanisms that progressively overwhelm natural anti-reflux defenses. Understanding these changes reinforces the importance of weight management as a primary intervention for obese GERD patients.