How is bacteriophage therapy being applied in clinical practice?
Bacteriophage therapy is being applied clinically through compassionate use programs, personalized treatment protocols, and combination therapies with antibiotics, showing promise for treating multidrug-resistant infections that fail conventional therapy. This mini-review examines real-world applications and the practical considerations for implementing phage therapy in modern clinical practice.
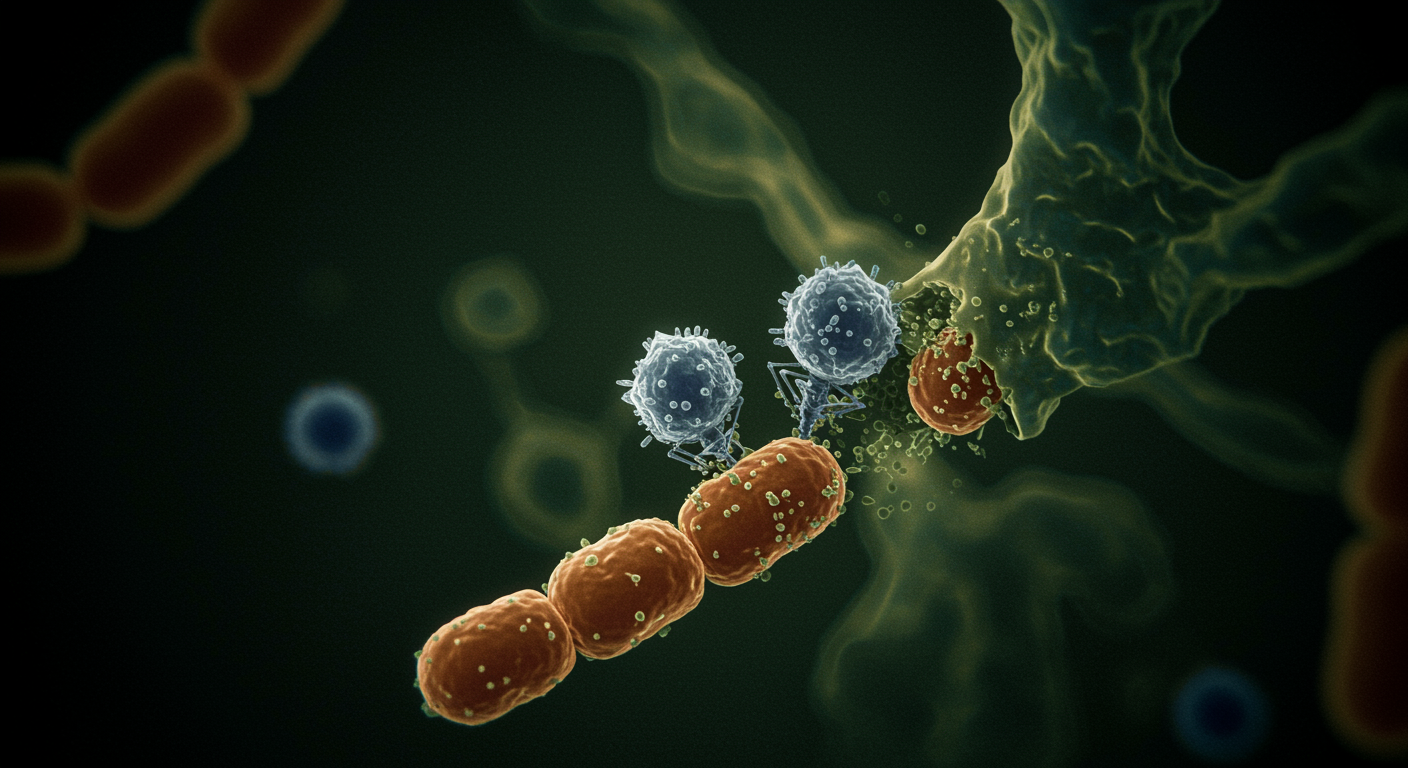
The clinical application of bacteriophage therapy represents a paradigm shift from traditional antimicrobial approaches, utilizing naturally occurring viruses that specifically target bacterial pathogens. Current clinical practice involves careful phage selection, personalized treatment protocols, and close monitoring for both efficacy and safety.
This clinical application connects to themes from the penicillin podcast about innovative approaches to treating infections, showing how the resistance challenges that followed antibiotic success are driving exploration of pre-antibiotic therapeutic concepts adapted for modern medical practice.
What the data show:
- Compassionate use programs provide access: Phage therapy is being used for critically ill patients with multidrug-resistant infections when conventional treatments have failed
- Personalized protocols are essential: Treatment requires careful selection of phages based on individual bacterial isolates and infection characteristics
- Combination approaches show promise: Phage therapy combined with antibiotics may provide synergistic effects and prevent resistance development
- Safety profiles are encouraging: Clinical experience suggests phage therapy has favorable safety profiles with minimal adverse effects
This mini-review provides insights into the practical application of bacteriophage therapy in clinical settings, examining current protocols, patient selection criteria, and the integration of this biological approach into modern medical practice.
Dr. Kumar’s Take
The clinical application of phage therapy shows how desperate clinical need can drive adoption of innovative approaches even before they’re fully validated through traditional clinical trials. The compassionate use programs demonstrate both the promise of this approach and the urgent need for alternatives to failing antibiotics.
What strikes me most is how phage therapy requires a completely different clinical mindset - from selecting chemical compounds to choosing living organisms, from standardized treatments to personalized protocols. This biological approach to antimicrobial therapy represents a fundamental shift in how we think about treating infections.
Historical Context
Phage therapy was first used clinically in the early 20th century but was largely abandoned in Western medicine after antibiotics became available. The current clinical revival reflects growing recognition that some multidrug-resistant infections cannot be treated with available antibiotics.
Modern clinical applications benefit from advanced microbiological techniques for phage characterization, genomic sequencing for safety assessment, and sophisticated monitoring capabilities that weren’t available during phage therapy’s early era.
What the Research Shows
The mini-review reveals several important aspects of current clinical phage therapy applications:
Compassionate Use Programs Phage therapy is being provided to critically ill patients with multidrug-resistant infections through compassionate use protocols when conventional treatments have failed, providing valuable clinical experience.
Personalized Treatment Protocols Clinical applications require careful selection of phages based on bacterial susceptibility testing, infection site characteristics, and patient-specific factors, representing a precision medicine approach.
Combination Therapy Strategies Clinical experience suggests that combining phages with antibiotics may provide synergistic effects, potentially overcoming resistance mechanisms and preventing the development of phage resistance.
Safety and Tolerability Clinical reports indicate favorable safety profiles with minimal adverse effects, though long-term safety data remain limited due to the relatively recent revival of clinical applications.
Monitoring and Optimization Clinical protocols include sophisticated monitoring for bacterial resistance development, phage persistence, and treatment response, enabling real-time optimization of therapy.
Practical Takeaways
- Personalized approaches are essential: Phage therapy requires individualized treatment protocols based on specific bacterial isolates and patient factors
- Combination strategies show promise: Combining phages with antibiotics may provide synergistic effects and prevent resistance development
- Safety profiles are encouraging: Clinical experience suggests favorable tolerability, though long-term data are still limited
- Regulatory pathways are evolving: Compassionate use programs are providing clinical experience while formal regulatory frameworks develop
Related Studies and Research
- Penicillin: The Accidental Discovery That Changed Medicine and Won a War
- Current Status of Clinical Trials for Phage Therapy
- Global Burden of Bacterial Antimicrobial Resistance
- 2019 Antibiotic Resistance Threats Report
FAQs
How are patients selected for phage therapy?
Patients typically have multidrug-resistant infections that have failed conventional antibiotic therapy, with phage selection based on bacterial susceptibility testing and infection characteristics.
What clinical conditions are being treated with phage therapy?
Current applications include respiratory infections, urinary tract infections, wound infections, and prosthetic joint infections caused by multidrug-resistant bacteria.
How is phage therapy administered to patients?
Administration routes include intravenous, topical, inhalation, and direct instillation depending on the infection site, with dosing protocols adapted from research studies and clinical experience.
What are the main safety considerations?
Safety monitoring includes assessment for immune reactions, bacterial resistance development, and potential effects on normal bacterial flora, though clinical experience suggests favorable safety profiles.
Bottom Line
Bacteriophage therapy is being successfully applied in clinical practice through compassionate use programs and personalized treatment protocols, showing promise for treating multidrug-resistant infections that fail conventional therapy. The clinical experience demonstrates favorable safety profiles and the potential for combination approaches with antibiotics. While regulatory frameworks continue to evolve, current clinical applications are providing valuable insights into the practical implementation of this biological approach to antimicrobial therapy, representing a significant paradigm shift in treating resistant infections.