Does H. Pylori Infection Actually Protect Against Barrett’s Esophagus?
Yes, Helicobacter pylori infection significantly reduces the risk of Barrett’s esophagus by 44% according to this comprehensive meta-analysis. The protective effect appears to result from H. pylori-induced reduction in gastric acid production, which decreases the severity of acid reflux that drives the development of Barrett’s metaplasia in the esophagus.
Dr. Kumar’s Take
This meta-analysis reveals another fascinating paradox of H. pylori infection - while it can cause ulcers and gastric cancer, it actually protects against Barrett’s esophagus and esophageal adenocarcinoma. The mechanism makes biological sense: H. pylori reduces acid production, which means less severe reflux and lower risk of the chronic acid exposure that leads to Barrett’s changes. This creates a complex clinical dilemma about H. pylori treatment in certain patients and highlights how our understanding of “good” and “bad” bacteria continues to evolve.
What the Research Shows
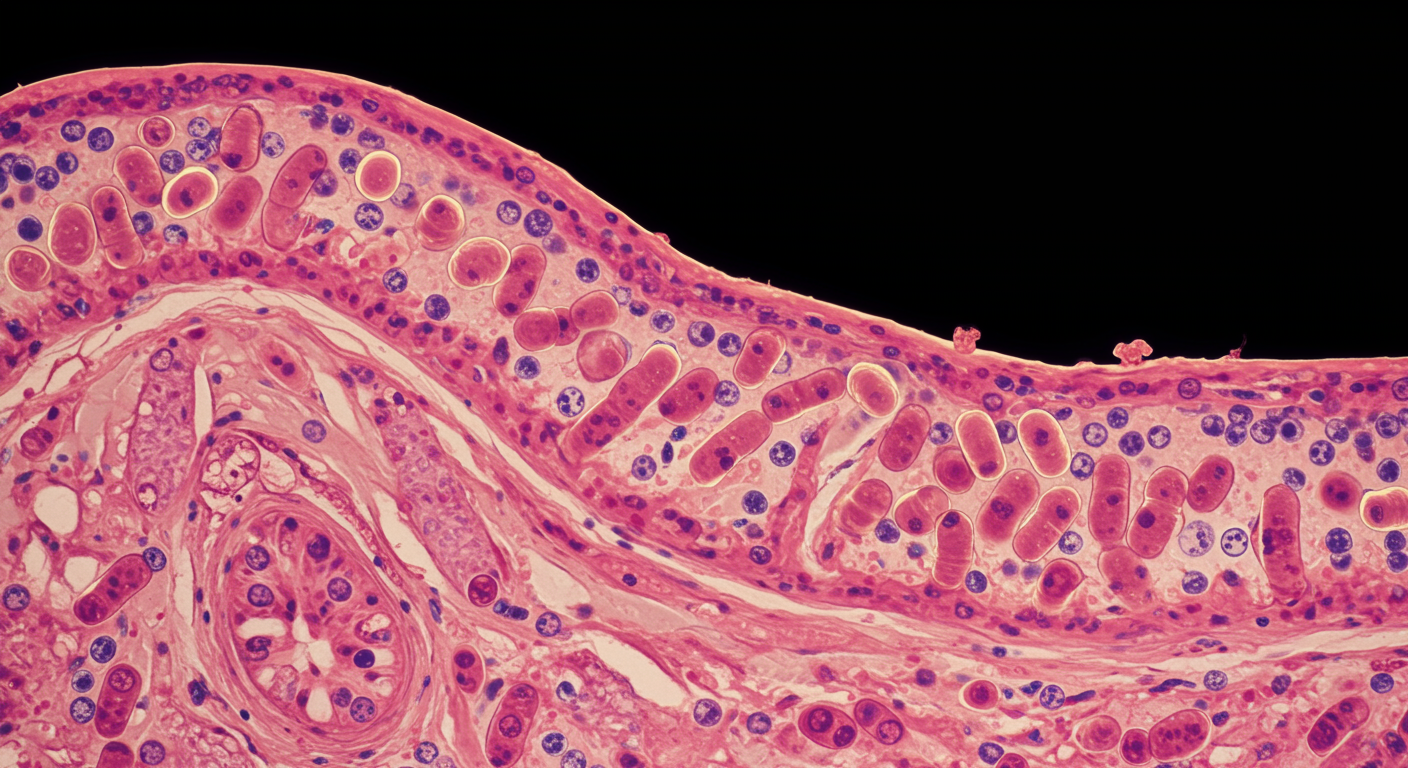
This systematic review and meta-analysis examined multiple studies investigating the relationship between H. pylori infection and Barrett’s esophagus risk. The analysis included case-control studies, cross-sectional studies, and cohort studies from various geographic regions to provide robust evidence for this protective association.
The research demonstrated a consistent inverse relationship between H. pylori infection and Barrett’s esophagus across different study designs and populations, suggesting a genuine protective effect rather than statistical artifact.
Study Snapshot
The meta-analysis included 26 studies encompassing over 8,000 Barrett’s esophagus cases and 20,000 controls from North America, Europe, Asia, and Australia. Studies used various methods to diagnose H. pylori infection and employed standardized criteria for Barrett’s esophagus diagnosis through endoscopy and histology.
Results in Real Numbers
- Overall Barrett’s esophagus risk reduction: 44% lower with H. pylori infection (OR 0.56, 95% CI 0.46-0.68)
- Geographic consistency: Protective effect seen across all continents studied
- Study type consistency: Similar protection in case-control and cross-sectional studies
- Dose-response relationship: Stronger protection with more virulent H. pylori strains
- Age effects: Protection more pronounced in older patients (>50 years)
- Gender differences: Slightly stronger protective effect in men than women
Safety, Limits, and Caveats
The meta-analysis was limited by heterogeneity in H. pylori detection methods, Barrett’s esophagus diagnostic criteria, and potential confounding factors across studies. The research couldn’t determine whether H. pylori eradication increases Barrett’s esophagus risk or assess the optimal timing of treatment decisions.
Additionally, the protective effect against Barrett’s esophagus must be weighed against H. pylori’s established risks for peptic ulcer disease and gastric adenocarcinoma, making treatment decisions complex and individualized.
Practical Takeaways
- Consider H. pylori status when evaluating Barrett’s esophagus risk in GERD patients
- Recognize that H. pylori eradication might theoretically increase Barrett’s esophagus risk in some patients
- Individualize H. pylori treatment decisions based on patient age, family history, and overall risk profile
- Monitor GERD symptoms and consider enhanced surveillance after H. pylori eradication in high-risk patients
- Understand that the protective effect doesn’t eliminate Barrett’s esophagus risk entirely
- Discuss the complex risk-benefit profile of H. pylori infection with patients when making treatment decisions
Related Studies and Research
- Gastroesophageal Reflux Disease and Helicobacter Pylori: What May Be the Relationship?
- Physiology, Stomach
- Current Advancement on the Dynamic Mechanism of Gastroesophageal Reflux Disease
- Global Prevalence and Risk Factors of Gastroesophageal Reflux Disease
- Episode 25: The Great GERD Mistake - How Medicine Made Heartburn Worse and How to Fix It
FAQs
Should I avoid treating H. pylori if I’m at risk for Barrett’s esophagus?
Treatment decisions should be individualized based on your overall risk profile, family history, and symptoms - discuss the complex risk-benefit analysis with your healthcare provider.
Does this mean H. pylori infection is beneficial?
While H. pylori may protect against Barrett’s esophagus, it also increases risks of ulcers and gastric cancer, so the overall health impact depends on individual circumstances.
Can H. pylori eradication increase my Barrett’s esophagus risk?
Theoretically possible, though not definitively proven - patients may need enhanced GERD monitoring and treatment after H. pylori eradication.
How does H. pylori protect against Barrett’s esophagus?
The protection likely results from H. pylori-induced reduction in gastric acid production, which decreases the severity of acid reflux that drives Barrett’s development.
Should Barrett’s esophagus patients be tested for H. pylori?
H. pylori testing may be appropriate as part of comprehensive evaluation, though treatment decisions require careful consideration of individual risk factors and expert consultation.
Bottom Line
Helicobacter pylori infection reduces Barrett’s esophagus risk by 44% through acid suppression mechanisms. This protective effect adds complexity to H. pylori treatment decisions and highlights the need for individualized risk-benefit assessments in clinical practice.