Why Don’t We Fully Understand How Estrogen Protects Blood Vessels?
Despite decades of research showing that estrogen has protective effects on blood vessels, many fundamental questions remain unanswered. We know estrogen improves endothelial function, reduces inflammation, and promotes healthy blood flow, but the precise mechanisms and why timing matters so much for cardiovascular benefits are still being unraveled by researchers.
Dr. Kumar’s Take
This research highlights why hormone therapy decisions are so complex and why individualized care is essential. We have compelling evidence that estrogen protects blood vessels when given at the right time to the right women, but we’re still learning exactly how this works. This uncertainty has contributed to the confusion around hormone therapy’s cardiovascular effects, but it shouldn’t prevent women from accessing treatment when the evidence supports benefits.
What the Research Shows
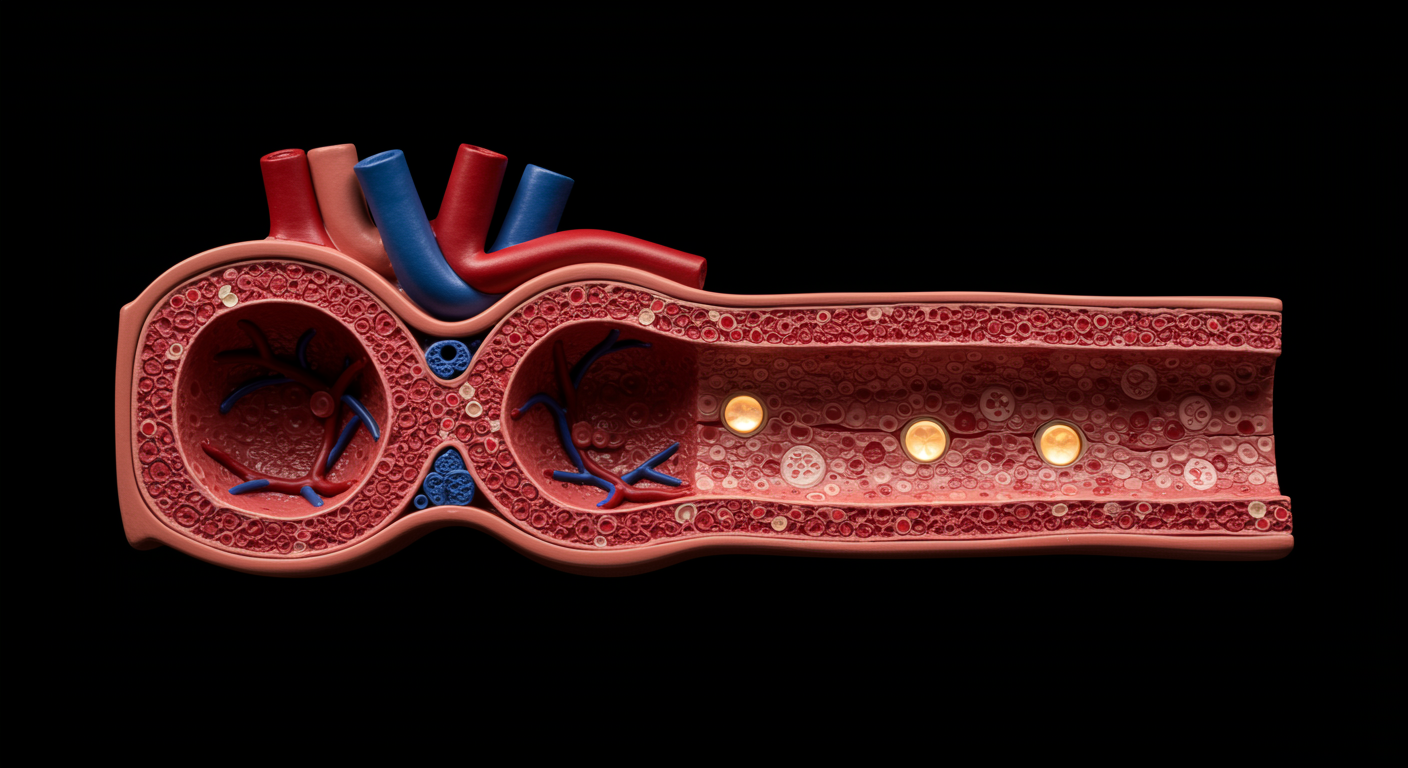
Studies consistently demonstrate that estrogen has multiple beneficial effects on the vascular system, including improved endothelial function, enhanced nitric oxide production, reduced oxidative stress, and anti-inflammatory effects. However, the timing hypothesis suggests these benefits are most pronounced when estrogen is started during perimenopause or early menopause. The mechanisms underlying this timing-dependent effect remain incompletely understood, creating ongoing research questions about optimal treatment strategies.
How This Works (Biological Rationale)
Estrogen acts on blood vessels through multiple pathways involving estrogen receptors in endothelial cells. It promotes nitric oxide synthesis, which helps blood vessels relax and maintain healthy blood flow. Estrogen also reduces inflammatory markers and oxidative stress that contribute to atherosclerosis. However, when blood vessels already have established disease, estrogen may have different effects, potentially explaining why older women in the WHI didn’t see cardiovascular benefits. The exact molecular mechanisms governing these age and timing-dependent effects are still being investigated.
Practical Takeaways
- Understand that estrogen’s cardiovascular effects are complex and timing-dependent, which explains conflicting research findings
- Recognize that starting hormone therapy during perimenopause or early menopause may provide cardiovascular benefits
- Know that individual factors like existing cardiovascular disease, genetics, and overall health status influence estrogen’s vascular effects
- Consider that ongoing research may refine our understanding of optimal hormone therapy timing and formulations
- Seek providers who understand the nuanced relationship between estrogen and cardiovascular health
- Don’t let scientific uncertainty prevent appropriate treatment when evidence supports benefits for your individual situation
What This Means for Perimenopause and Menopause Care
The ongoing questions about estrogen’s vascular effects highlight the importance of individualized care and shared decision-making. While we don’t have all the answers, we have enough evidence to support hormone therapy for appropriate candidates, particularly younger, healthier women starting treatment during the menopausal transition. This research underscores why women deserve access to providers who understand the complexity of these decisions rather than blanket recommendations based on incomplete understanding.
Related Studies and Research
- The Effects of Menopause Hormone Therapy on Lipid Profile in Postmenopausal Women
- Effects of menopause on temperature regulation
- Association of Menopausal Hormone Therapy With Breast Cancer Incidence and Mortality
- Recurrent Urinary Tract Infection in Older Outpatient Women
- Episode 27: Perimenopause, Menopause, and HRT - What Every Woman Should Know
FAQs
If we don’t fully understand how estrogen affects blood vessels, is hormone therapy safe?
While questions remain about precise mechanisms, we have substantial evidence about estrogen’s effects and can make informed decisions based on current knowledge, individual risk factors, and timing of treatment initiation.
Why does timing matter so much for estrogen’s cardiovascular effects?
Healthy blood vessels appear to respond differently to estrogen than diseased vessels. Starting treatment when vessels are still healthy (during perimenopause) may provide protection, while starting later may not offer the same benefits.
Will future research change hormone therapy recommendations?
Ongoing research will likely refine our understanding and may lead to more personalized approaches based on individual cardiovascular risk profiles, genetics, and optimal timing strategies.
Bottom Line
While important questions remain about exactly how estrogen protects blood vessels, current evidence supports cardiovascular benefits when hormone therapy is started appropriately. The complexity of these effects underscores the importance of individualized care and shared decision-making with knowledgeable providers.