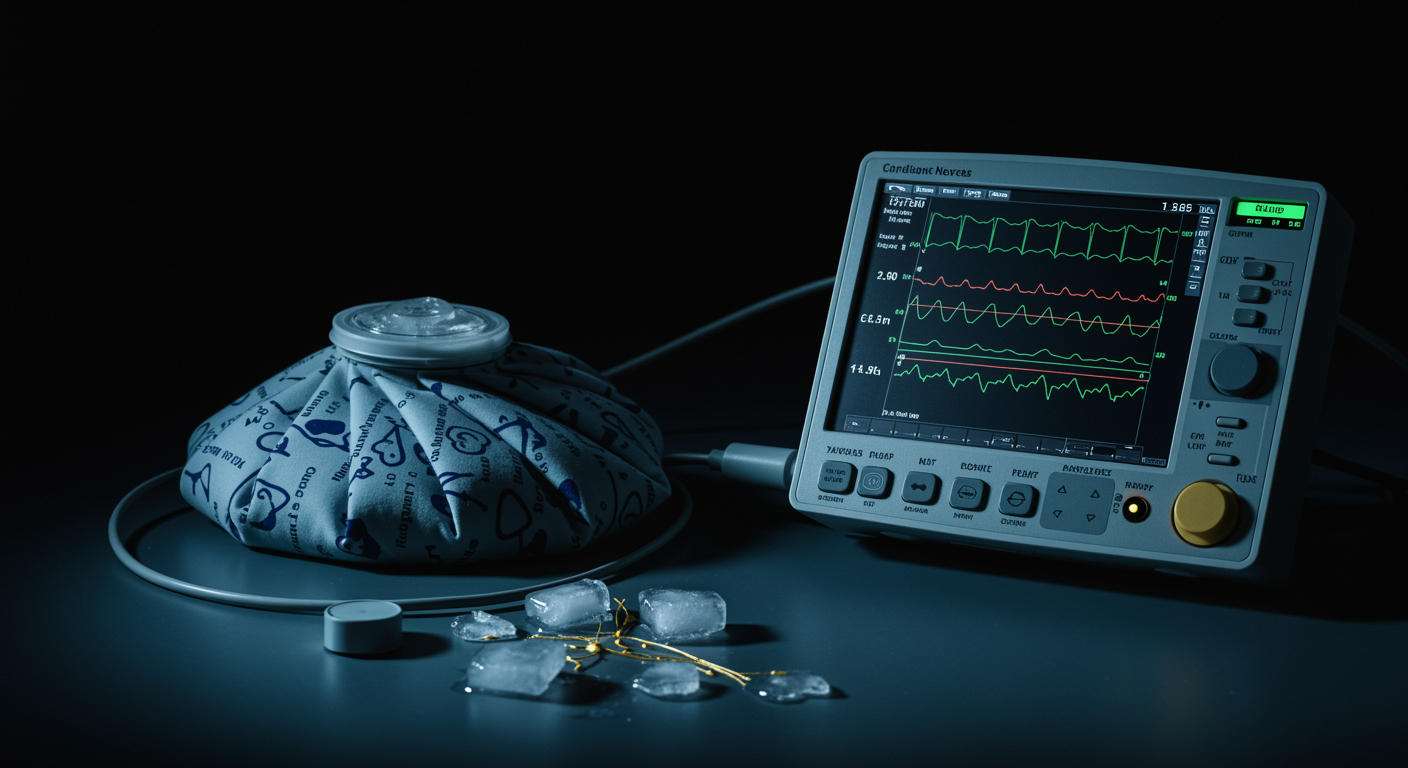
Can Applying Cold to Your Neck Reduce Stress?
Yes. This randomized controlled trial found that cold stimulation to the lateral neck significantly increased heart rate variability and decreased heart rate, suggesting activation of the body’s relaxation response. The neck region showed the strongest effect compared to the cheek and forearm.
Researchers from the University of Luxembourg wanted to find out if localized cold exposure could trigger the body’s calming vagus nerve. They were exploring the potential for a wearable device that could help people reduce stress in real-time. The results suggest the lateral neck is an effective target area.
Dr. Kumar’s Take
This study is fascinating because it points toward practical stress-relief technology. Rather than requiring a full ice bath or cold shower, targeted cold application to the neck could activate the body’s relaxation response. The researchers are thinking ahead to wearable devices that could sense stress and apply cooling automatically. While more research is needed, this is an exciting first step toward technology-assisted stress management.
Study Design
The study used a randomized, within-participant design with 61 healthy volunteers. Researchers applied cold stimulation using a thermode device (a temperature-controlled plate) to three body locations on the right side:
- Lateral neck
- Cheek
- Forearm
Each location received cold stimulation in 16-second intervals over 4 trials. The control condition used the same procedure but kept the temperature at baseline (no cooling). Researchers measured heart rate and heart rate variability using electrocardiogram recordings.
Key Findings
The results showed a clear pattern of cardiovascular response to cold stimulation:
Neck showed the strongest effect: Cold stimulation to the lateral neck produced significantly higher heart rate variability and lower heart rate compared to the control condition.
Location matters: The effect was specific to body location. The researchers found both a main effect and an interaction effect for body location and condition for both heart rate and heart rate variability measurements.
Suggests vagal activation: The pattern of increased heart rate variability with decreased heart rate points to activation of the vagus nerve, which controls the body’s relaxation response.
Why the Neck?
The lateral neck region is rich in nerve pathways connected to the vagus nerve and the diving reflex system. When cold receptors in this area are stimulated, they can trigger a cascade of relaxation responses:
- Slowing of heart rate
- Increased heart rate variability (a sign of healthy stress adaptation)
- Activation of the parasympathetic nervous system (the “rest and digest” system)
This is similar to what happens during the diving reflex, when cold water on the face triggers the body to conserve oxygen.
Implications for Stress Relief
The researchers designed this study with wearable technology in mind. Modern stress is often:
- Sudden and unpredictable
- Occurring in settings where exercise or meditation isn’t practical
- Requiring immediate intervention rather than delayed solutions
A wearable device that could detect elevated stress (through heart rate monitoring) and apply targeted cooling to the neck could provide real-time stress relief without requiring behavioral changes or private space.
Practical Takeaways
- Cold applied to the lateral neck can activate the body’s relaxation response
- The effect appears quickly (within seconds of cold application)
- This approach might work when you can’t use other stress-relief methods
- A cold pack or cooling device on your neck may help during stressful moments
Related Studies and Research
- Related Podcast Episode
- Plasma catecholamines and serotonin metabolites during a winter swimming season (PDF)
- Dose-response style synthesis: duration/temperature “dose” of CWI
- Sea swimming as a novel intervention for depression and anxiety
- Effects of adding facial immersion to chest-level water immersion on vmHRV
FAQs
How cold does the stimulation need to be?
The study used a thermode device to apply controlled cold, but didn’t specify exact temperatures in the available abstract. Future studies will need to test different temperatures and durations to find the optimal settings.
Can I use this technique at home?
While this study used specialized equipment, you could try applying a cold pack to the side of your neck during stressful moments. Start gently and avoid excessive cold that could cause discomfort.
How long does the effect last?
The study used 16-second cold applications. The duration of the relaxation effect after cold is removed needs further research, as does whether repeated applications provide cumulative benefits.
Bottom Line
This randomized controlled trial demonstrates that cold stimulation to the lateral neck can significantly increase heart rate variability and decrease heart rate in healthy adults. These changes suggest activation of the vagus nerve and the body’s relaxation response. The neck appears to be a particularly effective target area, more so than the cheek or forearm. This research opens the door to developing wearable stress-relief technology that could provide real-time cooling intervention. Future studies need to test different temperatures, durations, and stress conditions.