Dr. Kumar’s Take
This study shows us that our gut health isn’t just about the type of microbes you have but where they live and how they’re arranged. The colon works like a layered factory called a bioreactor, and S. boulardii helps preserve its architecture during the upheaval caused by strong antibiotics. For patients, that spatial resilience may be what protects against lasting damage.
Key Takeaways
- Antibiotic treatment with ciprofloxacin + metronidazole suppresses many bacterial groups; most suppression occurs in the central fermentative region of the stool cylinder.
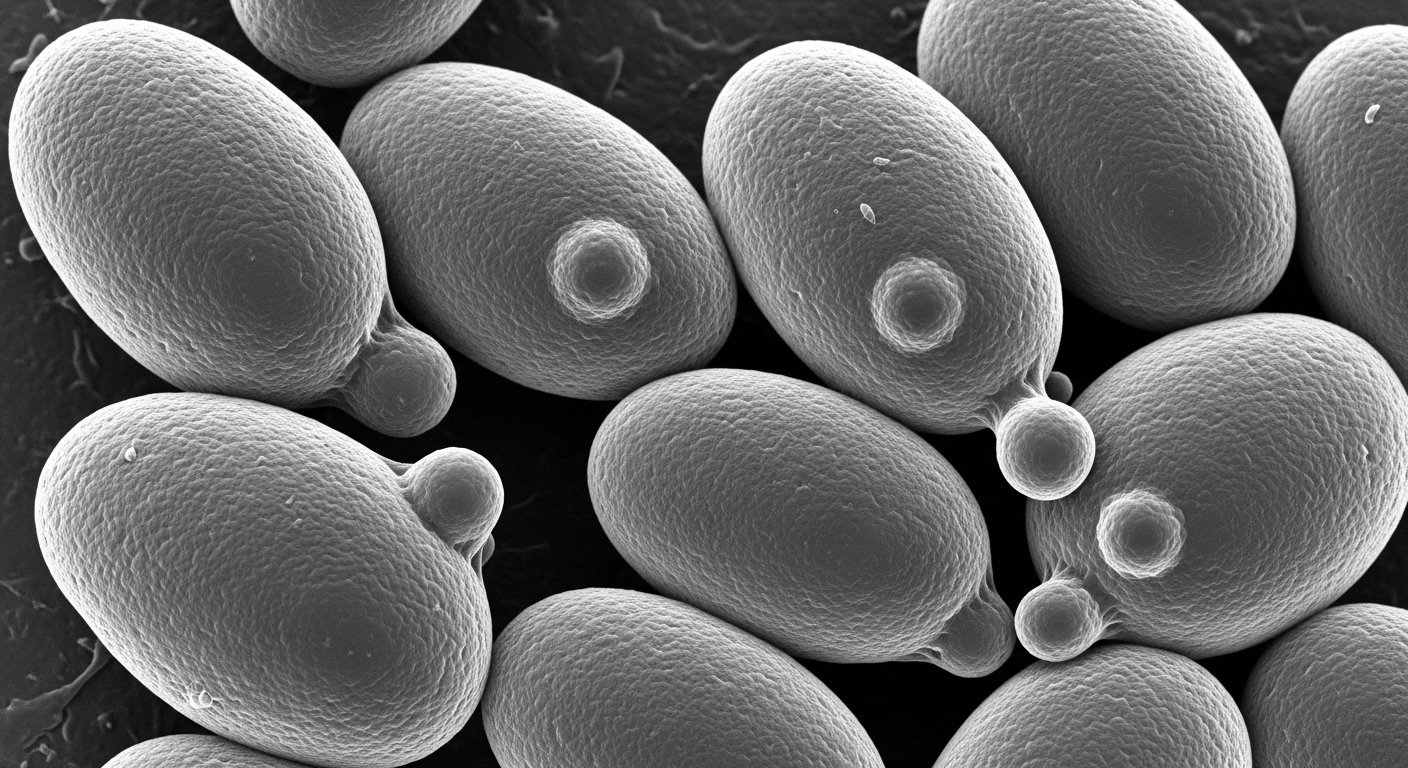
- There are three key zones in the “colonic bioreactor”: an outer mucus layer with almost no bacteria, a transitional mucus layer rich in bacteria, and a fermentation area inside largely filled with bacterial biomass and digestive leftovers.
- S. boulardii given concomitantly or prophylactically reduces antibiotic-induced suppression of “essential” bacterial groups (e.g. Faecalibacterium prausnitzii, Bacteroides, Roseburia).
- Recovery of bacterial diversity and biomass is much faster and more complete in S. boulardii‑treated groups, though even with probiotic treatment, full recovery takes months.
- Spatial location matters: the transitional layer acts like a refuge during antibiotic insult, and recovery tends to spring from there.
Actionable Tip
When prescribing strong antibiotics, consider starting Saccharomyces boulardii CNCM I‑745 at the same time. Supporting the structure of gut microbiota matters just as much as bacterial composition.
Study Summary
Swidsinski et al. studied women treated for bacterial vaginosis who received a two‑week antibiotic course (ciprofloxacin plus metronidazole), either with or without S. boulardii. They analyzed stool “cylinders” using fluorescence‑in‑situ hybridization (FISH) to map where bacterial groups lived across mucus and fermentative zones, and tracked recovery over months after therapy.
Study Design
- Population: 60 women (three groups of ~20 each) undergoing treatment for bacterial vaginosis
- Intervention Groups:
- Antibiotics alone
- Antibiotics + S. boulardii given during antibiotics (concomitant)
- S. boulardii given after antibiotics (prophylactic post‑course)
- Antibiotic Regimen: Ciprofloxacin + Metronidazole, 14 days
- Measurements: Stool cylinders collected before, during, and after treatment; FISH used to examine ~180 bacterial groups; focus on bacterial biomass, diversity, spatial arrangement (mucus layers, fermentative core)
- Follow‑up Duration: Up to ~130‑160 days (about 4–5 months) after antibiotic cessation
Results
- “Essential” bacterial groups were strongly suppressed by antibiotics, especially in the central fermentation (inner) zone.
- Many species retreated to the transitional mucus layer, which showed less suppression.
- In groups receiving S. boulardii (during or after), suppression was less severe and recovery of both biomass and diversity was faster.
- By ~3‑4 months, S. boulardii groups had regained much of their bacterial concentrations and many bacterial species; antibiotic‑only group remained below baseline.
- Spatial recovery started in the transitional mucus layer, with bacterial migration into the fermentative core over time.
Biological Rationale
- The outer mucus layer acts as a barrier/zone with few bacteria, which likely protects deeper layers from washout.
- Transitional mucus layer is enriched with bacteria and seems to serve as a “seed zone” or refuge: when antibiotics hit, many bacteria survive here, enabling repopulation.
- S. boulardii helps preserve these bacteria, likely through supporting mucosal integrity, modulating microbe‑mucus interactions, perhaps influencing host immune responses or competition so essential taxa don’t collapse completely.
Strengths & Limits
Strengths:
- Deep spatial mapping of bacterial distribution, which many studies overlook.
- Long follow‑up (~4–5 months), allowing observation of slower recovery dynamics.
- Multiple treatment arms (during and after) to compare prophylactic vs concurrent use of S. boulardii.
Limitations:
- Only female participants with bacterial vaginosis; generalizability to other populations (men, children, other antibiotic regimens) is unproven.
- FISH mapping captures a large number of groups but may miss rarer or non‑probed taxa.
- Recovery incomplete even with S. boulardii in some bacterial groups; functional implications (symptoms, metabolism) not deeply tested in this paper.
Related Studies and Research
- Saccharomyces boulardii in the prevention of antibiotic-associated diarrhoea: meta‑analysis
- Saccharomyces boulardii in the prevention of antibiotic-associated diarrhoea in children: RCT
- SB + Amoxicillin‑Clavulanate Effects on Gut Microbiota (RCT)
- High‑Dose Vancomycin + SB for Recurrent C. difficile
- 🎙️ Saccharomyces boulardii Explained – Podcast Episode
FAQ
Does the study suggest we should always give S. boulardii concurrently with antibiotics or is post‑antibiotic useful?
Both regimens showed benefit; concomitant use reduced suppression most strongly, while post‑antibiotic prophylaxis helped speed recovery when antibiotics were finished.
How long until the gut microbiota structurally recovers after a strong antibiotic course?
Even with S. boulardii, full or near‑full recovery in this study took about 3–5 months. Without it, recovery lagged and some essential groups remained below baseline.
Are there symptoms measured in this study (diarrhea etc.)?
This work focused on bacterial architecture, biomass, and diversity rather than clinical symptoms. However, preserving structure is likely to reduce risk of dysbiosis‑related symptoms.
Bottom Line
Strong antibiotics severely disrupt both the species and the physical structure of the gut microbiota. Saccharomyces boulardii, especially when given during or immediately after antibiotic courses, helps preserve the colon’s layered architecture (especially the transitional mucus layer), supports the survival of essential bacterial groups, and accelerates recovery. Structural protection may underlie probiotic benefits beyond mere species count.