How Significant Is Hiatal Hernia for GERD and Overall Health?
Hiatal hernia has significant clinical importance, particularly for gastroesophageal reflux disease, as it disrupts the normal anatomical barriers that prevent acid reflux. While many small hiatal hernias are asymptomatic, larger hernias substantially increase GERD risk and severity, and may require specific treatment approaches beyond standard acid suppression therapy.
Dr. Kumar’s Take
Hiatal hernia represents a perfect example of how anatomy affects function in GERD. While not everyone with a hiatal hernia develops severe reflux, it’s a major risk factor that changes how we approach treatment. Large hernias often don’t respond well to medications alone and may need surgical repair. The key is understanding that hiatal hernia isn’t just an incidental finding - it’s often the underlying anatomical problem driving persistent GERD symptoms.
What the Research Shows
This comprehensive clinical review examined the relationship between hiatal hernia and various gastrointestinal conditions, with particular focus on GERD pathophysiology and treatment outcomes. The analysis included endoscopic studies, manometric evaluations, and long-term follow-up data to assess the clinical significance of different hernia types and sizes.
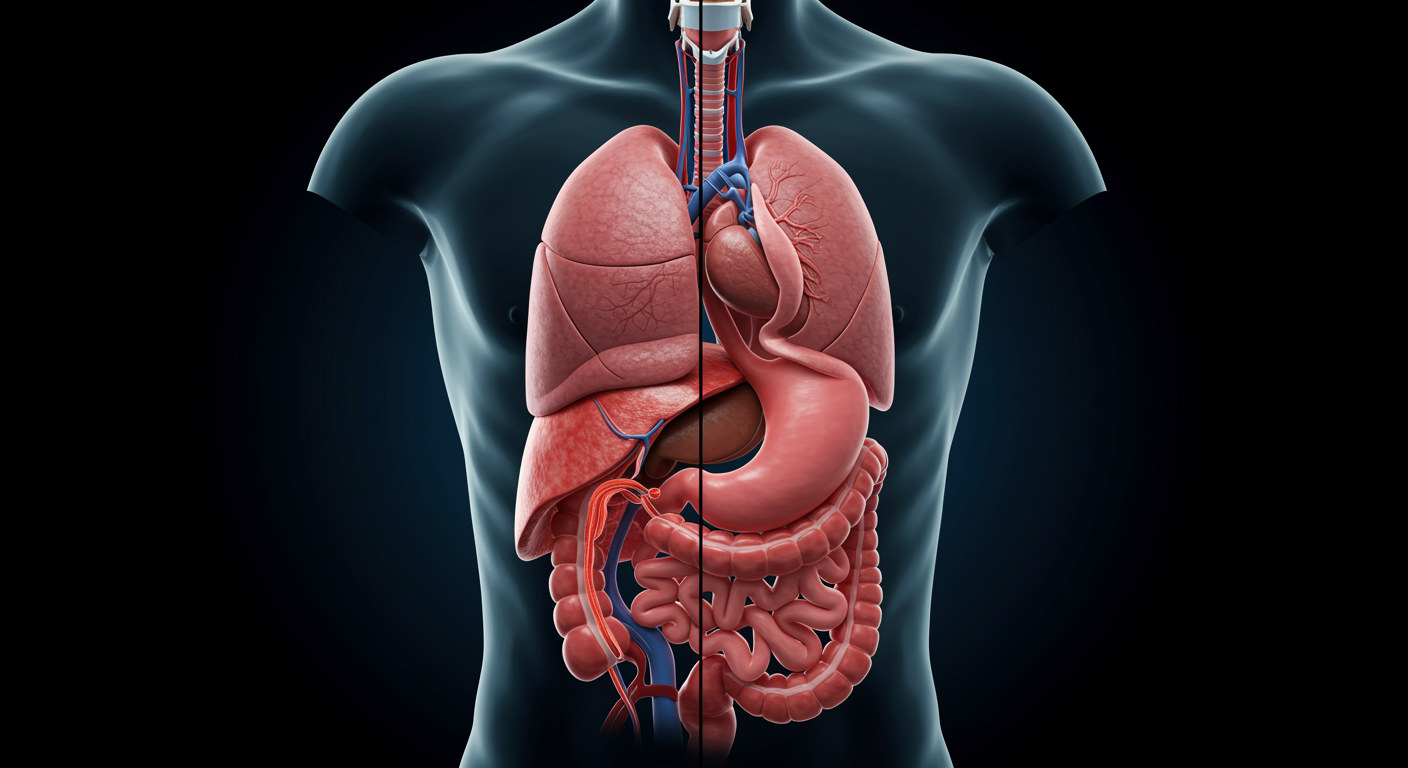
The research demonstrates that hiatal hernia significantly impairs the gastroesophageal junction’s ability to prevent reflux through multiple mechanisms including loss of the angle of His, reduced lower esophageal sphincter pressure, and impaired esophageal clearance of refluxed material.
Study Snapshot
The review analyzed clinical data from multiple endoscopic and manometric studies involving thousands of patients with varying degrees of hiatal hernia. Researchers examined correlations between hernia size, GERD severity, treatment response, and long-term outcomes across different patient populations and treatment modalities.
Why This Matters for Health and Performance
Understanding hiatal hernia’s clinical significance helps explain why some GERD patients don’t respond well to standard medical therapy and may need surgical intervention. It also provides insight into the anatomical basis of reflux disease, helping patients understand that their symptoms may have a structural component requiring specific treatment approaches.
Recognition of hiatal hernia’s role in GERD can prevent unnecessary medication escalation and guide appropriate referrals for surgical evaluation when medical therapy fails to provide adequate symptom control.
Safety, Limits, and Caveats
The clinical significance of hiatal hernia varies considerably between individuals, with some patients having large hernias but minimal symptoms while others have small hernias with severe GERD. The relationship between hernia size and symptom severity isn’t always linear, and other factors like obesity, diet, and lifestyle significantly influence clinical outcomes.
Diagnostic accuracy for hiatal hernia can vary depending on the imaging method used, and the clinical relevance of small, sliding hernias remains debated among gastroenterologists and surgeons.
Practical Takeaways
- Recognize that hiatal hernia may explain persistent GERD symptoms despite optimal medical therapy
- Consider surgical evaluation for patients with large hiatal hernias and refractory reflux symptoms
- Understand that lifestyle modifications remain important even with hiatal hernia-associated GERD
- Monitor patients with hiatal hernia more closely for GERD complications like Barrett’s esophagus
- Educate patients that hiatal hernia represents an anatomical problem that may require surgical correction
- Avoid unnecessary medication escalation when anatomical factors are the primary driver of symptoms
Related Studies and Research
- Hiatal Hernia, Lower Esophageal Sphincter and Their Combined Effect
- Association Between Obesity and GERD: A Review of the Epidemiological Evidence
- Global Prevalence and Risk Factors of Gastroesophageal Reflux Disease
- The Effects of Modifying Amount and Type of Dietary Carbohydrate on Esophageal Acid Exposure
- Episode 25: The Great GERD Mistake - How Medicine Made Heartburn Worse and How to Fix It
FAQs
Can hiatal hernia cause symptoms other than heartburn?
Yes, hiatal hernia can cause chest pain, difficulty swallowing, shortness of breath, and in large hernias, early satiety and nausea due to stomach displacement into the chest cavity.
Do all hiatal hernias require surgery?
No, many small hiatal hernias are asymptomatic and require no treatment. Surgery is typically considered for large hernias causing severe symptoms or complications that don’t respond to medical therapy.
Can hiatal hernia develop over time or is it present from birth?
Most hiatal hernias are acquired over time due to factors like aging, increased abdominal pressure, obesity, and weakening of the diaphragmatic muscles, though some may have congenital predisposition.
How is hiatal hernia diagnosed?
Hiatal hernia is typically diagnosed through upper endoscopy, barium swallow studies, or CT scans, with endoscopy being the most common method during GERD evaluation.
Can lifestyle changes help with hiatal hernia symptoms?
Yes, weight loss, smaller meals, avoiding late eating, and head elevation can significantly improve symptoms even when hiatal hernia is present - consult your healthcare provider for personalized recommendations.
Bottom Line
Hiatal hernia has significant clinical importance, particularly for GERD patients, as it represents an anatomical disruption of normal anti-reflux mechanisms. Understanding its role helps guide appropriate treatment decisions and explains why some patients may need surgical intervention beyond medical therapy.