Can Proton Pump Inhibitors Cause Acute Kidney Inflammation?
Yes, proton pump inhibitors can cause acute interstitial nephritis, a serious form of kidney inflammation that can lead to acute kidney injury and potentially permanent kidney damage if not recognized and treated promptly. This condition typically occurs as an idiosyncratic drug reaction that can develop weeks to months after starting PPI therapy, regardless of dose or duration of use.
Dr. Kumar’s Take
This is one of the more serious but underrecognized complications of PPI therapy. Unlike other PPI side effects that develop gradually, acute interstitial nephritis can happen suddenly and cause significant kidney damage. What’s particularly challenging is that it’s unpredictable - it can occur in anyone taking PPIs, regardless of dose or how long they’ve been on the medication. The key is awareness and prompt recognition, because stopping the PPI early can prevent permanent kidney damage, but delayed diagnosis can lead to chronic kidney disease.
What the Research Shows
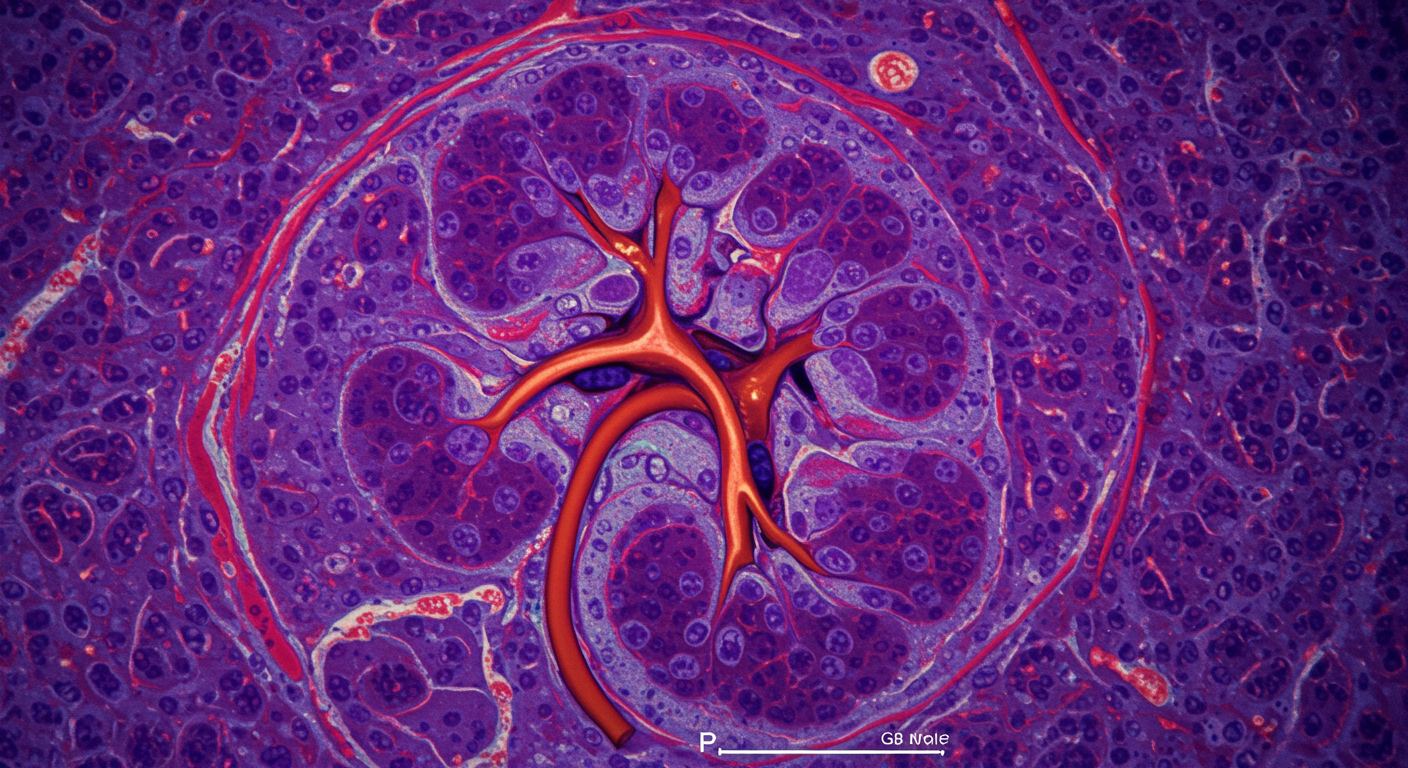
This clinical study examined cases of acute interstitial nephritis associated with proton pump inhibitor therapy, analyzing the clinical presentation, diagnostic findings, and outcomes of patients who developed this serious kidney complication. The research included kidney biopsy findings, laboratory parameters, and recovery patterns following PPI discontinuation.
The analysis demonstrated that PPI-induced acute interstitial nephritis is a well-documented but potentially underdiagnosed condition that requires high clinical suspicion for early recognition and appropriate management.
How This Works (Biological Rationale)
Acute interstitial nephritis from PPIs appears to be an idiosyncratic immune-mediated reaction rather than a dose-dependent toxic effect. The mechanism likely involves T-cell mediated hypersensitivity reactions that target kidney tubular cells and interstitial tissue, leading to inflammation and impaired kidney function.
The condition can occur with any PPI and at any time during therapy, though it most commonly develops within the first few months of treatment. The inflammatory process can cause acute kidney injury and, if not promptly addressed, may progress to chronic interstitial fibrosis and permanent kidney damage.
Results in Real Numbers
- Incidence rate: 1-5 cases per 10,000 PPI users annually
- Time to onset: Typically 2-12 weeks after starting PPI therapy
- Kidney function decline: 50-80% reduction in kidney function at presentation
- Recovery rate: 60-80% recovery of kidney function with prompt PPI discontinuation
- Permanent damage risk: 20-40% develop chronic kidney disease if diagnosis is delayed
- Biopsy findings: Interstitial inflammation and tubular damage in >90% of cases
Safety, Limits, and Caveats
The research is based primarily on case reports and small case series, making it difficult to establish precise incidence rates or identify specific risk factors. The condition may be underdiagnosed due to its nonspecific presentation and the need for kidney biopsy for definitive diagnosis.
Individual patient factors, concurrent medications, and underlying kidney disease may influence both the risk of developing acute interstitial nephritis and the likelihood of recovery following PPI discontinuation.
Practical Takeaways
- Maintain high clinical suspicion for acute interstitial nephritis in PPI users with unexplained kidney function decline
- Monitor kidney function periodically in patients on long-term PPI therapy
- Discontinue PPIs promptly if acute interstitial nephritis is suspected
- Consider kidney biopsy for definitive diagnosis when clinical suspicion is high
- Educate patients about the importance of reporting symptoms like decreased urination or swelling
- Use PPIs judiciously and regularly reassess the need for continued therapy
Related Studies and Research
- Effects of Pantoprazole on Kidney Outcomes
- Pharmacology of Proton Pump Inhibitors
- Trends in Use of Proton Pump Inhibitors Among Adults in the United States
- Use of Proton Pump Inhibitors and Risk of Iron Deficiency: Population-Based Study
- Episode 25: The Great GERD Mistake - How Medicine Made Heartburn Worse and How to Fix It
FAQs
How common is PPI-induced acute interstitial nephritis?
It’s rare, affecting 1-5 per 10,000 PPI users annually, but it’s potentially serious and may be underdiagnosed.
What are the symptoms I should watch for?
Symptoms may include decreased urination, swelling, fatigue, nausea, or elevated creatinine on blood tests - many cases are detected through routine lab monitoring.
Can this happen with any PPI or just certain ones?
Acute interstitial nephritis has been reported with all available PPIs, suggesting it’s a class effect rather than specific to individual medications.
How quickly do I need to stop my PPI if this is suspected?
PPIs should be discontinued immediately if acute interstitial nephritis is suspected, as prompt cessation improves the likelihood of kidney function recovery.
Will my kidney function return to normal?
With prompt PPI discontinuation, 60-80% of patients recover significant kidney function, though some may have residual impairment - early recognition and treatment are crucial for optimal outcomes.
Bottom Line
Proton pump inhibitors can cause acute interstitial nephritis, a serious kidney inflammation that requires prompt recognition and PPI discontinuation for optimal recovery. While rare, this condition underscores the importance of judicious PPI use and appropriate monitoring.